Translate this page into:
Comparison of pupil dilation in manual small incision cataract surgery using topical versus intracameral mydriatic agents – A randomised controlled trial
*Corresponding author: Ibukunoluwa James Adeogun, Department of Ophthalmology, Lagos State University Teaching Hospital, Ikeja, Lagos, Nigeria. ibkciti@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Adeogun IJ, Adekoya BJ, Balogun MM. Comparison of pupil dilation in manual small incision cataract surgery using topical versus intracameral mydriatic agents – A randomised controlled trial. Glob J Cataract Surg Res Ophthalmol. 2024;3:4-9. doi: 10.25259/GJCSRO_2_2024
Abstract
Objectives:
The purpose of this research is to assess and compare the efficacy of an intracameral mydriatic solution with conventional topical agents in the completion of manual small incision cataract surgery (MSICS) in a black population.
Materials and Methods:
This randomised controlled trial was conducted among 102 patients undergoing MSICS under sub-tenon’s block. Mydriasis in the topical group was achieved with a pre-operative topical dilating combination of tropicamide 0.8% and phenylephrine 5% while surgery was commenced in patients in the intracameral group without dilation, and mydriasis was achieved intraoperatively with an intracameral solution of lidocaine 0.5% and adrenaline 0.001%. Pupil sizes were measured serially, before, and at four different junctures during surgery. The proportion of patients needing supplementary mydriasis in either group was noted, as well as post-operative pinhole visual acuity (VA). Data analysis was carried out using the Statistical Package for the Social Sciences Statistical Product and Service Solutions(SPSS) version 25.0 (IBM, Chicago, Illinois). The level of statistical significance was set at P < 0.05 at a 95% confidence interval.
Results:
Mean pupil diameter before dilating and blocking was 2.5 ± 0.6 mm in the topical group and 2.5 ± 0.7 mm in the intracameral group (P = 0.752). This increased to 7.7 ± 1.1 mm and 7.4 ± 0.8 mm, respectively (P = 0.134), after administering either mydriatic agents. After that, mean pupil diameter progressively reduced in both groups but was significantly higher in the intracameral group at each point of measurement (P < 0.05). Postoperatively, there was no significant difference in the VA between the two groups (P < 0.05).
Conclusion:
Using an intracameral mixture of lidocaine and adrenaline gives adequate mydriasis for the successful completion of MSICS without pre-operative dilation.
Keywords
Cataract
Pupil
Intracameral mydriatic
Topical mydriatic
INTRODUCTION
Cataract is a major cause of blindness globally,[1] although reversible. The treatment for cataract is surgical extraction, and this is the most commonly performed surgery worldwide. Of the many techniques of cataract surgery that have evolved, two predominate globally – Phacoemulsification and manual small incision cataract surgery (MSICS).
Whatever the method of cataract surgery, a major factor in the completion of a successful procedure is pupil size. Adequate pupillary dilation is essential for the safe completion of cataract surgery and for reducing the incidence of complications. Optimal capsulorrhexis/capsulotomy, lens nucleus delivery, cortical washout, and intraocular lens (IOL) insertion are all dependent on a well-dilated pupil. When this is inadequate, there is an increased occurrence of tissue damage, retained lens matter, posterior capsular rent, and vitreous loss.[2]
Conventionally, mydriasis for cataract surgery has been achieved by repeated pre-operative instillation of topical anticholinergic and sympathomimetic agents such as tropicamide 1%, cyclopentolate 1%, and phenylephrine 2.5% or 10%.[3] More recent methods include the use of a mydriatic-soaked cellulose pledget, which is inserted into the inferior conjunctival fornix 60 min before surgery.[4] Pre-operative adjunctive use of topical non-steroidal anti-inflammatory drugs such as diclofenac, ketorolac, and flurbiprofen has also been proven to aid the maintenance of mydriasis intraoperatively.[5-7]
Nevertheless, these methods do not come without their disadvantages. Pre-operative dilation of the pupil has been associated with drawbacks such as a need for additional manpower and resources – a nurse is often dedicated to the repeated instillation of the eyedrops into patients’ eyes; increased patient preparation time, the possibility of ocular surface toxicity from the preservative present in most eyedrops and the possible non-compliance with pre-operative mydriatic drops among day-case patients.[8] In addition, iris problems such as intraoperative floppy iris syndrome and iris fatigue, which occur from repeated instillation of topical mydriatic agents, are also common with topical mydriasis.[9-11] Furthermore, pupil response to topical mydriatics is particularly prolonged in darkly pigmented irides compared to the light-coloured ones.[12] Increased systemic absorption with attendant cardiovascular adverse effects of some of these medications, though rare, has also been documented.[13]
The challenges mentioned above can be creditably avoided if mydriasis can be initiated intraoperatively. Many studies have examined the use of various intracameral agents solely in the induction and maintenance of mydriasis during phacoemulsification and found it to be as effective as the pre-operative topical agents.[14-16] However, the efficacy of these agents has been scarcely explored globally for the MSICS procedure. Doing a PubMed search, only one article was found to have studied the efficacy of intracameral agents in intraoperative initiation and maintenance of mydriasis in MSICS.[8] No such study was found to have been conducted in Africa.
MATERIALS AND METHODS
This study was conducted at the Lagos State University Teaching Hospital, a tertiary centre in Lagos, Nigeria. Ethical approval was obtained from the Hospital’s Ethics and Research Committee before the commencement of the study. Written informed consent was also obtained from each participant. The study was designed as a prospective randomised controlled trial and registered with the Pan African Clinical Trials Registry (PACTR); registration number – PACTR202011892936115.
Adult patients with uncomplicated cataracts scheduled for MSICS were recruited for this study. Exclusion criteria included patients aged <18 years, pregnant or breastfeeding women, history of uveitis, history of intake of alpha-blockers, use of topical or systemic non-steroidal anti-inflammatory drugs/prostaglandins/miotics, presence of corneal opacities or pupillary deformities, history of surgery in the same eye and hypersensitivity to any component of medicines used. Furthermore, patients who did not attain pupillary dilatation of at least 7 millimetre (mm) during the pre-operative review and those that had intraoperative complications that can interfere with the pupil diameter, such as vitreous loss and iridodialysis were excluded from the study.
All recruited patients had slit-lamp examination done and cataract was graded using the lens opacification classification system version III;[17] intraocular pressure was also measured.
Randomisation into the two groups was achieved on surgery day using the Sequentially Numbered Opaque and Sealed Envelope technique.[18] Patients randomised into the topical group underwent pupillary dilation using pre-operative topical eyedrop containing tropicamide 0.8% and phenylephrine 5% (Appamide plus, Appasamy Associates, India) applied at 15 min intervals one hour before surgery. Patients in the intracameral group received no pre-operative dilating drops. They received a solution of adrenaline 0.001% and preservative-free lidocaine 0.5% prepared as follows: 0.2 millilitre (mL) of adrenaline 0.1% (Epinephrine, Wuhan Grand Pharmaceuticals, China) was diluted to 10 mL with normal saline to make a concentration of 0.002%. 2 mL of this solution was then diluted with an equal volume of lidocaine 1% (Oculan, Sunways, India) to make a solution containing lidocaine and adrenaline at 0.5% and 0.001% concentrations, respectively.
Each patient underwent MSICS under sub-tenon anaesthesia. The anaesthetic solution was a 5 mL solution comprising 2 mL of bupivacaine 2% (Duracaine, Myunsung Pharmaceuticals, China), 2.5 mL of lidocaine 1% (C-zocaine, Bharat Parenterals, India), and 0.5 mL of hyaluronidase (Hyanidase, Shreya Life Sciences, India).
On the day of surgery, after completing the randomisation process, patients underwent MSICS. A baseline pupil diameter, P1, was measured with Castroviejo callipers by the principal investigator before the instillation of topical mydriatic in the mydriatic group and just before giving local anaesthetic block in the intracameral group. Other pupil diameter measurements were taken by the operating surgeon at four time-points during the surgery. P2 was measured 30 s after injection of the mydriatic solution in the intracameral group and 1 min after anterior chamber (AC) entry with the keratome in the topical group. P3 was measured just after nucleus delivery for both groups. The fourth pupil diameter reading, P4, was taken just before IOL insertion after injecting viscoelastic, and the final measurement, P5, was made just before speculum removal at the end of the surgery. Additional intracameral mydriasis at any point during surgery was achieved by injection of 0.3 mL of adrenaline 0.001% and was noted by the research assistant. This was given when deemed necessary by the operating surgeon.
Data management
All data analysis was carried out using the software – Statistical Product and Service Solutions (SPSS) version 25 (IBM, Chicago, Illinois). Categorical variables were presented using frequencies and percentages. Continuous variables were presented as mean ± standard deviation, while median and interquartile values were used when skewed. Kolmogorov– Smirnov test was used to assess normal distribution for numeric data. Association between categorical variables was carried out using the Chi-square test or Fisher’s exact test. Mean comparisons were carried out using the Independent Student t-test, while median comparison was evaluated using the Mann–Whitney U-test. P <0.05 was accepted as statistically significant at a 95% confidence interval.
RESULTS
A total of 102 patients scheduled for MSICS were recruited for this study and were randomised into two groups of equal numbers based on the agent employed in achieving mydriasis.
Six patients, three in each group, were lost to follow-up in the course of the study. At three weeks postoperatively, number of participants was 50 and 49 in the topical and intracameral groups, respectively, while it was 48 each at six weeks postoperatively.
Sociodemography of participants
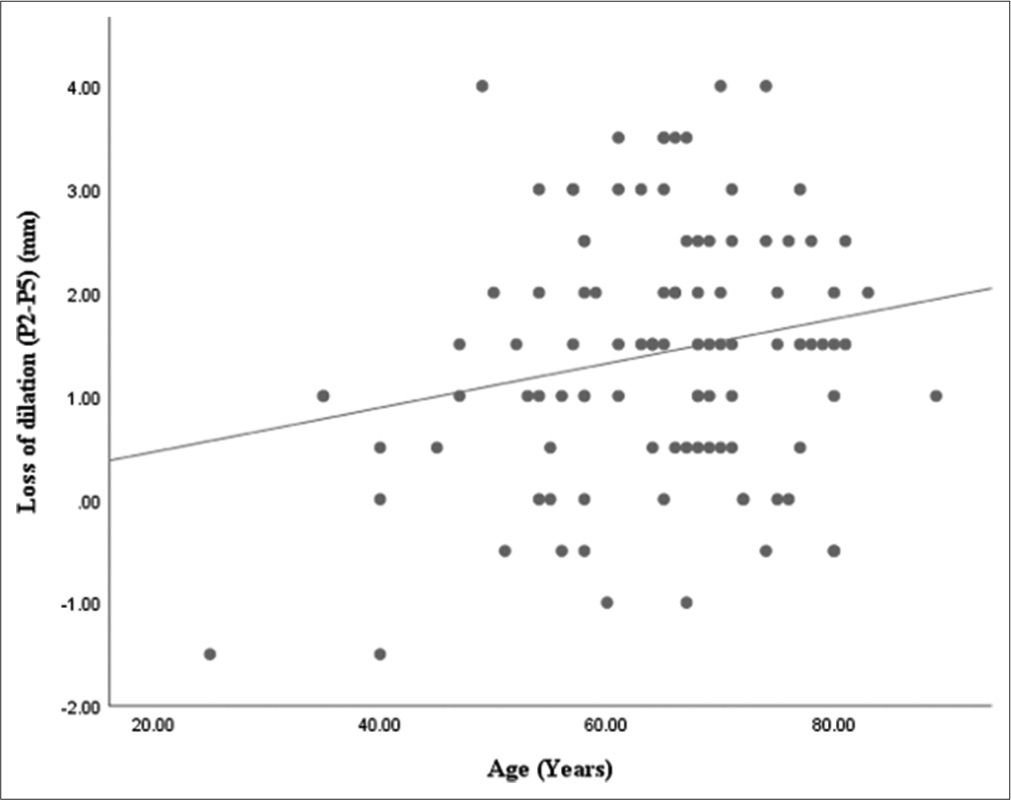
The age of the patients in this study ranged between 25 and 89 years, with mean ages of 64.9 ± 10.7 years and 66.6 ± 12.1 years in the topical and intracameral groups, respectively. Overall, there were no statistically significant differences between the sociodemographic characteristics of the topical and intracameral groups, as shown in Table 1. In general, the reduction in pupil dilation was proportional to increasing age, as shown in Figure 1 (Correlation coefficient = 0.199, P = 0.045).
| Variables | Topical (n=51) Freq (%) | Intracameral (n =51) Freq (%) | Total | χ2 | P-value |
|---|---|---|---|---|---|
| Age group (years) | |||||
| <50 | 6 (11.8) | 4 (7.8) | 10 (9.8) | 1.293* | 0.863 |
| 51-59 | 11 (21.6) | 8(15.7) | 19 (18.6) | ||
| 60-69 | 13 (25.5) | 16 (31.4) | 29 (28.4) | ||
| 70-79 | 15 (29.4) | 16 (31.4) | 31 (30.5) | ||
| >80 | 6 (11.8) | 7(13.7) | 13 (12.7) | ||
| Mean±SD | 64.9±10.7 | 66.6±12.1 | 0.782** | 0.590 | |
| Gender | |||||
| Male | 24 (47.1) | 23 (45.1) | 47 (46.1) | 0.039 | 0.849 |
| Female | 27 (52.9) | 28 (54.9) | 55 (53.9) | ||
| Educational level | |||||
| None | 12 (23.5) | 2 (3.9) | 14 (13.7) | 10.884* | 0.112 |
| Primary | 13 (25.5) | 21 (41.2) | 34 (33.3) | ||
| Secondary | 14 (27.5) | 20 (39.2) | 34 (33.3) | ||
| Tertiary | 12 (23.5) | 8(15.7) | 20 (19.7) | ||
- Relationship between loss of dilation and age of participants
Mean pupil diameter of participants
There was no difference between the mean baseline pupil diameters of each group. After dilation and AC entry, the mean pupil diameter was comparable at 7.7 ± 1.1 mm and 7.4 ± 0.8 mm in the topical and intracameral groups, respectively. Further into the surgery, the mean pupil diameter continued to decline in both groups. However, it was significantly larger in the intracameral group than in the topical group till the end of the surgery, as shown in Table 2.
| Topical (n =51) Mean±SD (mm) |
Intracameral (n =51) Mean±SD (mm) |
t-value | P-value | |
|---|---|---|---|---|
| P1 | 2.5±0.6 | 2.5±0.7 | 0.317 | 0.752 |
| P2 | 7.7±1.1 | 7.4±0.8 | 1.512 | 0.134 |
| P3 | 5.8±1.5 | 6.5±1.4 | -2.518 | 0.013* |
| P4 | 5.2±1.3 | 6.1±1.3 | -3.567 | 0.001* |
| P5 | 4.3±1.1 | 5.1±1.3 | -3.347 | 0.001* |
| % reduction from P2 to P5 | 44.3% | 31.1% | -6.054 | <0.001* |
Supplementary intraoperative mydriasis
In either group, only two patients received supplementation of mydriasis intraoperatively using 0.3 mL of 0.001% adrenaline solution. This is depicted in Figure 2:

- Proportion of cases needing further intraoperative mydriasis.
Pinhole visual acuity (VA)
The pre-operative median logMAR pinhole VA was −3.00 for both groups. On the 1st postoperative day and the 6th postoperative week, the median logMAR pinhole VA was better in the topical group, but the difference was not statistically significant, as shown in Table 3.
| Topical (n =51)* Median (Q1-Q3) | Intracameral (n =51)* Median (Q1-Q3) | U-value | P-value | |
|---|---|---|---|---|
| Preoperatively | -3.00 (-3.00, -2.00) | -3.00 (-3.00, -2.00) | -1.683 | 0.194 |
| 1 day post-operative | -0.48 (-0.78, -0.18) | -0.63 (-0.95, -0.35) | -0.539 | 0.590 |
| 1 week post-operative | -0.18 (-0.48, -0.18) | -0.18 (-0.41, 0.00) | -1.066 | 0.286 |
| 3 weeks post-operative | -0.18 (-0.48, -0.18) | -0.18 (-0.27, -0.05) | -0.561 | 0.575 |
| 6 weeks post-operative | 0.00 (-0.18, 0.00) | -0.18 (-0.18, 0.00) | -0.238 | 0.812 |
DISCUSSION
Sociodemography
The mean ages of patients in this study were comparable between both groups (P = 0.590). Females were more than males probably because they have better health-seeking behaviour. These findings are comparable with those of Ajay et al.[8] where mean ages in the topical and intracameral groups were 64.8 ± 8.3 years and 65.4 ± 8.6 years, respectively. Nikeghbali et al.[15] and Suan et al.[19] also reported mean ages close to the values observed in this study. In the studies mentioned above, females were also more than males.
Primary outcome
Baseline pupil diameter was similar between the topical and intracameral groups at 2.5 ± 0.6 mm and 2.5 ± 0.7 mm, respectively (P = 0.752). These were comparable to findings in a study by Nikeghbali et al.[15] in Iran, where the mean pupil diameters for the topical and intracameral groups were 2.50 ± 0.25 mm and 2.60 ± 0.33 mm, respectively, although the latter was done among patients who underwent phacoemulsification. In a similar study by Ajay et al. in India, the baseline pupil diameter for the topical group was measured after they had been dilated.[8] This is in contrast to what most other studies have done. The mean pre-dilation pupil diameter for the intracameral group was, however, higher (3.30 ± 0.6 mm) than recorded in this study. This could be due to racial differences or differences in the brightness of the ambient light in each study. After administering the anaesthetic block, pupil diameter barely increased by 0.3 mm in the topical group (dilating drop had already been instilled) but increased by 2.9 mm from baseline in the intracameral group. After entry into the AC, pupil diameter (P2) measurements in this study of 7.7 ± 1.1 mm (topical) and 7.4 ± 0.8 mm (intracameral) were not significantly different between groups (P = 0.134). Similarly, the mean pupil diameter in both groups was noted to have progressively decreased in the course of the surgery, probably due to the waning effect of the mydriatic agents. Furthermore, generally, reduction in pupil diameter correlated with increasing age as the surgery progressed, suggesting that older people are more responsive to miotic factors such as iris touch during MSICS.
However, the mean pupil diameter after P2 was significantly higher in the intracameral group than in the topical group (P < 0.005). This suggests that, although given at a lower dose, intracameral mydriatic agents attained a higher aqueous concentration than topical agents and thus could achieve longer-lasting effects over the operative period. In addition, in this study, there was a statistically significant difference (t = −6.054, P < 0.001) between the percentage reduction in mean pupil diameter from P2 to P5 (44.3% in the topical group and 31.1% in the intracameral group).
The above findings are similar to those of Ajay et al.[8] in India where mean pupil diameter reduced in both groups as surgery progressed but was significantly higher in the intracameral group after AC entry, although he measured the pupil diameter at six points in their study. Furthermore, the intraoperative reduction in mean pupil diameter was also significantly higher in the topical group.
In contrast, some other studies[14,19,20] reported that the mean pupil diameter progressively increased in the intracameral group while a decrease was noted in the topical group, although varying intracameral agents were used. Noteworthy in these studies is that a higher concentration of lidocaine (1%) was used intracamerally, and phacoemulsification was the surgery performed.
Secondary outcomes
VA
The differences in median pinhole visual acuities between both groups were not statistically significant (P > 0.005) on 1st post-operative day and throughout follow-up. This implies that the use of an intracameral mydriatic agent did not pose any characteristic sight-threatening complications postoperatively. It also gives further credence to its safety. These findings are similar to those of Ajay et al.[8] and Yu et al.[21]
Supplementary intraoperative mydriasis
In this study, 2 (3.9%) of the 51 patients in each group needed supplementary intracameral dilating agents. The patients in the topical group who required supplementation to aid nucleus delivery had pupil sizes of 4.0 mm and 4.5 mm. In the intracameral group, supplementary mydriasis was needed at the stage of IOL implantation, and pupil diameter was 4.5 mm in both. In the study by Ajay et al.,[8], only one patient in the intracameral group was deemed necessary for supplementary mydriasis – pupil size just before IOL implantation was 3 mm.
Slightly contrasting observations were documented by Nikeghbali et al.[15] where two patients (6%) in the topical group alone needed additional mydriasis at the time of IOL implantation due to pupil constriction and poor visibility of the capsular bag. In the Malaysian study by Suan et al.,[19] 6 patients (10.7%) in the topical group and 3 (5.4%) in the intracameral group required additional manoeuvres to achieve further mydriasis. The variation in these reports could be due to factors related to the surgeon’s techniques and preferences.
In all, between-group comparisons did not reveal statistically significant differences in the proportion of patients that needed supplementary mydriasis.
Limitations
The endothelial count was not studied in this study. This may have had an effect, especially in the intracameral group.
CONCLUSION
Intracameral mydriatics are practicable and efficacious alternatives to topical agents achieving adequate mydriasis for MSICS in a Nigerian population with expectedly satisfactory outcomes.
Acknowledgment
We are grateful to all of those who contributed to the success of this project, especially our research assistant and our department’s theatre staff.
Ethical approval
The research/study was approved by the Institutional Review Board at Lagos State University Teaching Hospital, number LREC/06/10/1437, dated 09-11-2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96:614-8.
- [CrossRef] [PubMed] [Google Scholar]
- Management of mydriasis and pain in cataract and intraocular lens surgery: Review of current medications and future directions. Clin Ophthalmol. 2014;8:1281-9.
- [CrossRef] [PubMed] [Google Scholar]
- Phacoemulsification without preoperative mydriasis in patients with age-related cataract associated with type 2 diabetes. Clin Ophthalmol. 2016;10:2427-32.
- [CrossRef] [PubMed] [Google Scholar]
- Use of a new ocular insert versus conventional mydriasis in cataract surgery. Biomed Res Int. 2013;2013:849349.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of topical nonsteroidal anti-inflammatory drugs on pupillary size during uncomplicated cataract surgery. J Refract Surg. 2017;33:236-42.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of the effect of topical bromfenac with nepafenac in maintaining mydriasis during cataract surgery. Delhi J Ophthalmol. 2015;26:97-100.
- [CrossRef] [Google Scholar]
- Effect of topical nonsteroidal anti-inflammatory drugs and nuclear hardness on maintenance of mydriasis during phacoemulsification surgery. J Ocul Pharmacol Ther. 2014;30:831-6.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of intraoperative intracameral mydriasis in manual small incision cataract surgery-a randomised controlled trial. Indian J Ophthalmol. 2017;65:584.
- [CrossRef] [PubMed] [Google Scholar]
- Intracameral phenylephrine to prevent floppy iris syndrome during cataract surgery in patients on tamsulosin. Eye. 2007;21:331-2.
- [CrossRef] [PubMed] [Google Scholar]
- Use of epinephrine for IFIS prophylaxis. J Cataract Refract Surg. 2006;32:1074-5.
- [CrossRef] [PubMed] [Google Scholar]
- Safety and efficacy of intracameral mydriatics: Lignocaine and epinephrine in manual small-incision cataract surgery and their effect on blood pressure and heart rate. Indian J Ophthalmol. 2021;69:1343-5.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluating the potentiating effect of amethocaine on tropicamide-induced mydriasis in darkly pigmented irides, using infrared pupillometry. Ophthalmol Eye Dis. 2014;6:13-9.
- [CrossRef] [PubMed] [Google Scholar]
- Systemic exposure to intracameral vs topical mydriatic agents: In cataract surgery. Clin Ophthalmol. 2019;13:805-9.
- [CrossRef] [PubMed] [Google Scholar]
- Phacoemulsification without preoperative topical mydriatics: Induction and sustainability of mydriasis with intracameral mydriatic solution. Indian J Ophthalmol. 2014;62:333-6.
- [CrossRef] [PubMed] [Google Scholar]
- Pupil dilation with intracameral lidocaine during phacoemulsification. J Cataract Refract Surg. 2007;33:101-3.
- [CrossRef] [PubMed] [Google Scholar]
- Optimizing the intracameral dilation regimen for cataract surgery: Prospective randomised comparison of 2 solutions. J Cataract Refract Surg. 2009;35:273-6.
- [CrossRef] [PubMed] [Google Scholar]
- The lens opacities classification system III. The longitudinal study of cataract study group. Arch Ophthalmol. 1993;111:831-6.
- [CrossRef] [PubMed] [Google Scholar]
- Randomization and allocation concealment: A practical guide for researchers. J Crit Care. 2005;20:187-91.
- [CrossRef] [PubMed] [Google Scholar]
- Intracameral mydriatics versus topical mydriatics in pupil dilation for phacoemulsification cataract surgery. J Cataract Refract Surg. 2017;43:1031-5.
- [CrossRef] [PubMed] [Google Scholar]
- Intracameral mydriatics in phacoemulsification cataract surgery. J Cataract Refract Surg. 2003;29:2366-71.
- [CrossRef] [PubMed] [Google Scholar]
- Pupil dilation with intracameral epinephrine hydrochloride during phacoemulsification and intraocular lens implantation. J Ophthalmol. 2016;2016:4917659.
- [CrossRef] [PubMed] [Google Scholar]







