Translate this page into:
Pseudo-plateau iris secondary to multiple peripheral pigment epithelial cysts: A case report
*Corresponding author: César Alas-Pineda, Department of Internal Medicine, Mario Catarino Rivas National Hospital, San Pedro Sula, Cortés, Honduras. cesar_alas10@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Argeñal Rodriguez RM, Alas-Pineda C, MolineroLeiva K, Pavón-Varela DJ, González Romero C. Pseudo plateau iris secondary to multiple peripheral pigment epithelial cysts: A case report. Glob J Cataract Surg Res Ophthalmol. 2025;4:44-7. doi: 10.25259/GJCSRO_28_2024
Abstract
Iris epithelial cysts are rare, spontaneous, epithelium-lined spaces that arise from the iris-pigmented epithelial layer and ciliary body and can cause a narrowing of the anterior chamber angle leading to a pseudo-plateau iris configuration (PPI). We present the case of an 80-year-old female patient with a history of decreased visual acuity, diagnosed with bilateral cataracts and pseudo-plateau iris secondary to multiple peripheral pigment cysts. This report describes the detection process, management strategy and course of treatment of a patient with bilateral cataracts who underwent cataract surgery by manual incision, and clinically presented with Pseudo-plateau iris secondary to Iris epithelial cyst. It highlights the importance of early detection and correct differentiation from malignant conditions, and anterior segment pathologies to prevent associated permanent complications.
Keywords
Angle-closure glaucoma
Cataracts
Iris cyst
Pseudo-plateau iris
INTRODUCTION
Iris epithelial cysts are rare, spontaneous and epithelium-lined spaces arising from the iris-pigmented epithelial layer and ciliary body can cause a narrowing of the anterior chamber angle, leading to a pseudo-plateau iris (PPI) configuration.[1,2] PPI represents an anterior displacement of the iris attachment secondary to a ciliary cyst, with or without angle-closure glaucoma. Although the exact prevalence of PPI is unknown, ciliary cysts are reported in 5–54% of healthy individuals.[2] It is often difficult to distinguish PPI between plateau iris (PI) since both can have an s-shaped configuration of the peripheral iris.[3] The importance of primary iris epithelial cysts lies in their similarities to iris or ciliary body neoplasms. Although they do not require treatment, they are rare, and their diagnosis and optimal management are a challenge when addressing other pathologies of the anterior segment.
CASE REPORT
The case report is of an 80-year-old female patient who has experienced a progressive decrease in visual acuity in both eyes, being more noticeable in the left eye, over a period of approximately 6 months. Regarding her medical history, the patient has a history of controlled arterial hypertension and a history of breast cancer, which was treated by a left mastectomy in 2011. To date, no recurrences have been reported and the results of the examinations of the lymph nodes have been negative. There is no history of eye trauma or other similar incidents.
During the initial examination, visual acuity was measured using the Snellen chart, yielding results of 20/60 in one eye and 20/400 in the other, both without correction. Bilateral intraocular pressure (IOP) measurement resulted in a value of 14 mmHg. Examination of the ocular adnexa revealed normal findings in both eyes. Subsequently, a detailed examination using a slit lamp was carried out to assess the anterior chamber and optic disc. The results show an anterior segment in the right eye with cataract classification NO2NC2 (Nuclear Opalescence Grade 2, Nuclear Color Grade 2) (LOCS III), the rest without alterations and cataract (NO4NC4C3) Nuclear Opalescence Grade 4, Nuclear Color Grade 4, Cortical Cataract Grade 3 (LOCS III) in the left eye [Figure 1], with a brown lesion in the temporal sector behind the iris between 2:00 and 6:00 h in the left eye, without transillumination [Figure 2]. Gonioscopy revealed a Grade 2 (20°) iridocorneal angle in both eyes; in addition, poor pharmacological mydriasis was observed after the application of 1% tropicamide plus 2.5% phenylephrine.
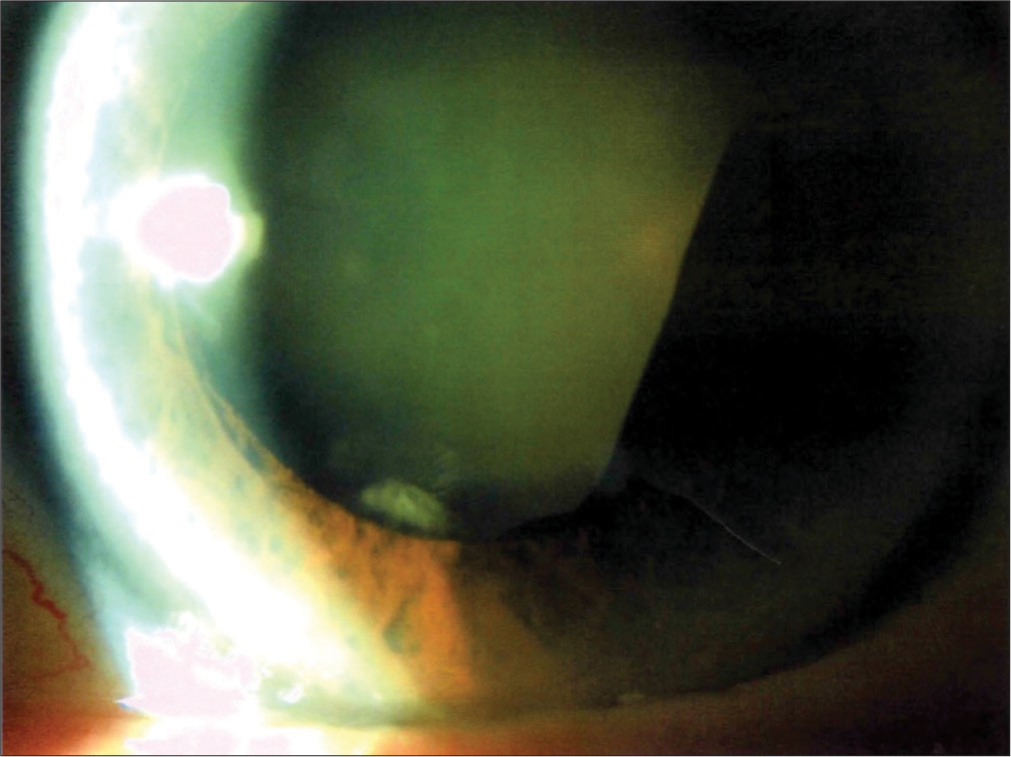
- Left eye, cataract.
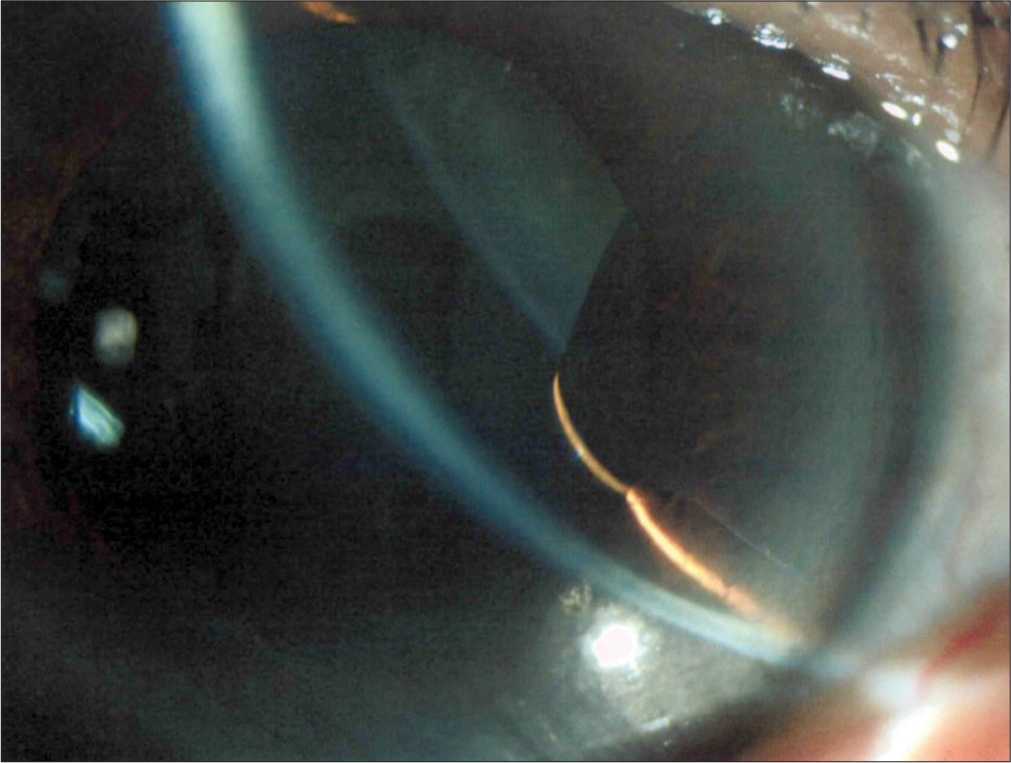
- Negative transillumination of the cyst.
Direct fundoscopy shows the excavation of 0.3, and the optic disc presented normal characteristics; cup-to-disc ratio was measured at 0.5 in each eye, indicative of a physiological cup within normal limits as well as the macula and the peripheral retina, although the presence of peripheral pigmentary degeneration was detected in the latter. Anterior segment optical coherence tomography (AS-OCT) shows an iris cyst posterior to the lens adjacent to the iris [Figure 3]. In the ultrasonic biomicroscopy (UBM) of the left eye, the ciliary body grooves were visible, except between 2:00 and 6:00 h, when the presence of a cyst of the iridociliary body that closed the grooves was evident [Figure 4]. This condition caused a narrowing and clogging of the angles, giving rise to an iris configuration that simulates a plateau but not completely, known as a PPI. The presence of a larger posterior iris peaking over the pupillary margin in an inferior temporal sectoral manner was noted [Figure 5]. A chain of cysts was also seen in the ciliary bodies, smaller in size compared to the previously mentioned cyst. No mass or abnormal vascularity was noted within the pars plana, ciliary body or iris.

- (a) Anterior segment optical coherence tomography. (b) Cyst of the iris posterior to the lens adjacent to the iris.

- (a) Ultrasonic biomicroscopy (UBM) of the plateau iris with iridociliary cysts (white arrow). (b) UBM of the left eye showing iridociliary cysts with a closed iridotrabecular angle (red arrow).
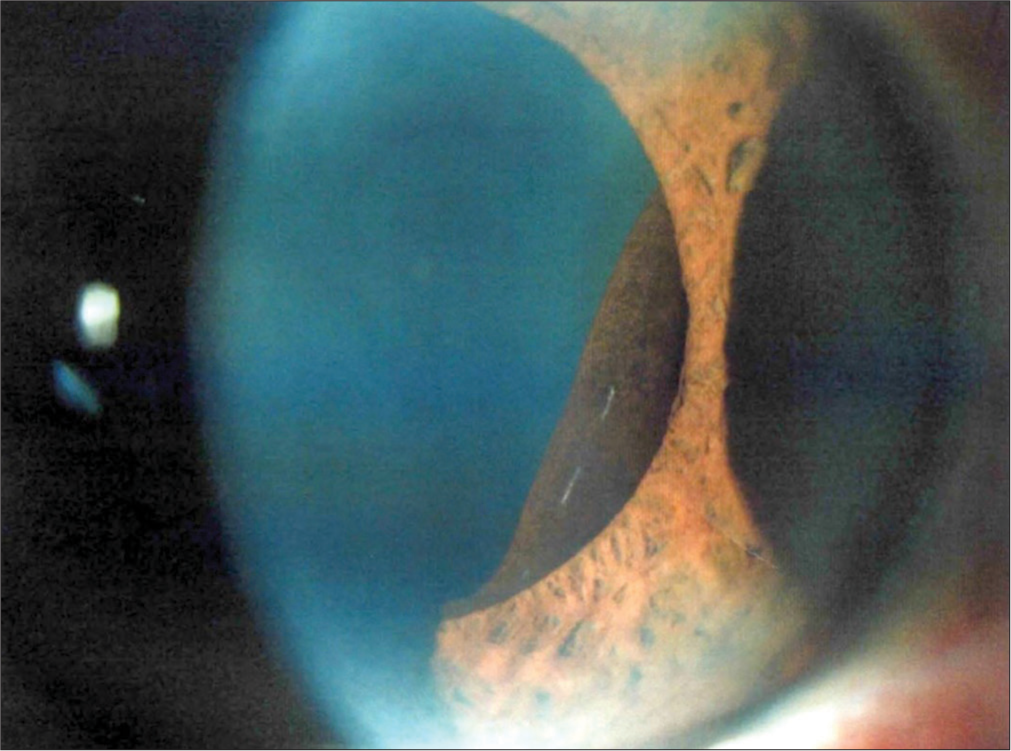
- Peripheral pigment epithelial cyst on the inferotemporal sectoral pupillary margin.
Surgical intervention was carried out for the management of the cataract using the small incision manual surgery technique due to the presence of poor pupillary dilation (mydriasis) and a high risk of bleeding from the iris cyst when pupillary dilation instruments are used. The patient was operated on successfully, with satisfactory evolution. This successful outcome showcases the benefits of the surgical technique, which effectively restored the patient’s visual function and quality of life.
DISCUSSION
Iris tumours can be classified as primary or secondary cysts.[4,5] Primary cysts generally originate from the posterior segment of the iris pigment epithelium and may be innocuous or present with secondary complications. These primary cysts are usually located in three specific areas: the pupillary margin (Central), between the root of the iris and the ciliary body (midzonal), and in the iridociliary groove (peripheral). Complications associated with primary cysts had been reported, such as corneal decompensation, uveitis, amblyopia, strabismus and secondary glaucoma.[5,6]
In this case, an enlargement of the posterior iris was observed, reaching its maximum point at the pupillary margin in a sectorial manner in the inferior temporal quadrant. This finding had been found consistently in previous studies, where embryological weakness in the inferior and temporal sectors due to the displacement of the internal and external layers of the optic cup is indicated as a pathogenic mechanism.[5,7,8] The literature reports cases of iridociliary cysts with and without angle-closure symptoms.[6,7] The area of involvement determined by the number of cysts present in the iridociliary groove could be an explanation for this complication. According to Marigo et al., it is usual to find a single cyst in the iridociliary groove, so the presence of multiple cysts is rare and would increase the probability of angle closure.[4,8]
A gonioscopy performed to assess the risk of angle closure revealed a Grade 2 (20°) iridocorneal angle in both eyes, indicating moderately narrow angles according to the gonioscopy classification system proposed by Schei[9] providing a 360° view of the anterior chamber angle from Schwalbe’s line to the ciliary body band.[8,10] It has been recommended to differentiate iris cysts with iris melanoma or ciliary body melanoma through clinical examination, UBM and AS-OCT.[10,11] UBM provides high-resolution images of the angular region and anterior chamber, essential for differentiating the cause of angle closure.[3,10,12]
In the left eye, UBM revealed that the ciliary body sulci were visible, except at 120°, where the iridociliary body cyst occluded the sulci. As a result, the angles narrow giving a PPI configuration, results consistent with studies suggesting that the mechanism of angle closure in a pseudo-plateau configuration was associated with multiple cysts in the iridociliary sulcus.[3,13] However, no mass or abnormal vascularity was seen within the pars plana, ciliary body, or iris. Therefore, it is concluded that it is a benign tumour and that the visual complications are mainly related to the presence of cataracts.
From a therapeutic perspective, different management strategies have been proposed, with the intensified approach being the most widely favoured in most cases. Different treatments have been reported to control ocular hypertension or glaucoma damage.[2,6,7,14-16] The current general protocol for treating angle closure is to lower IOP with medication and perform laser iridotomy. In patients with PPI secondary to iridociliary cysts, pharmacological mydriasis has shown results in IOP stabilisation, and the use of timolol 0.5% has been reported more frequently.[14] At present, the use of pilocarpine is infrequent and has been associated with poor patient adherence to treatment due to its dosing schedule of 3–4 times a day.[17] The use of prostaglandin analogues is recommended due to their effectiveness in lowering IOP in a single dose by increasing aqueous outflow through the uveoscleral pathway.[17] However, in this case, the IOP remained within normal values, and there were no clinical signs of angle-closure glaucoma, so no drug treatment was started for it. Andreatta et al. suggest 6 months of follow-up in patients with an acute attack of primary angle closure since IOP can increase during this period.[18]
It has been observed that there is a correlation between the duration of an acute attack of primary angle closure and the time in which symptoms are experienced and a greater probability of progression to primary angle-closure glaucoma.[18] Cataract surgery has been reported as an additional treatment used for primary angle closure.[15] Despite its high precision and safety, femtosecond laser-assisted cataract surgery has been controversial due to its high cost and results similar to those achieved by small-incision phacoemulsification as currently practiced.[19] However, in this case, the deficient pharmacological mydriasis of the pupil can make phacoemulsification difficult, having to use devices for small pupils such as rings and/or iris retractors. Due to the presence of an iridian cystine, the chances of bleeding from the use of these devices may increase and cause unnecessary complications. Due to the above and given that the decrease in the patient’s vision is secondary to the cataract, it was decided to use manual small incision cataract surgery as a surgical technique, showing a satisfactory evolution, obtaining a postoperative visual acuity of 20/25 a week after surgery, with normal IOP and no clinical data of glaucoma in the patient.
CONCLUSION
Primary epithelial cysts present a diagnostic challenge due to their resemblance to iris or ciliary body neoplasms. Despite the benign nature of this condition, its rarity underscores the importance of understanding its clinical presentation and optimal management, especially when considering anterior segment pathologies. Using accurate methods and interventions is mandatory to prevent permanent damage to patients’ vision due to glaucoma or IOP complications. This particular case highlights the significance of early detection and correct differentiation from malignant conditions to preclude unnecessary interventions. In addition, it underscores the importance of adapting surgical strategies to effectively address associated complications and promote satisfactory outcomes in visual function and quality of life for patients affected by this rare condition.
Acknowledgements
The authors would like to thank all the peer reviewers and editors for their opinions and suggestions.
Ethical approval
The research/study approved by the Catholic University of Honduras “Our lady queen of peace” San Pedro and San Pablo Campus research Ethics Committee, number EXP #2023008, dated 15th August 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Iris cysts: Varied presentations and review of literature. Saudi J Ophthalmol. 2021;35:341-6.
- [CrossRef] [Google Scholar]
- Asymmetric glaucoma in pseudoplateau iris syndrome. BMJ Case Rep. 2017;2017:bcr2017221141.
- [CrossRef] [Google Scholar]
- Clinical features distinguishing angle closure from pseudoplateau versus plateau iris. Br J Ophthalmol. 2008;92:340-4.
- [CrossRef] [Google Scholar]
- Plateau iris secondary to iridociliary cysts. Arch Soc Esp Oftalmol. 2015;90:542-5.
- [CrossRef] [Google Scholar]
- Primary iris cysts: A review of the literature and report of 62 cases. Br J Ophthalmol. 1984;68:152-66.
- [CrossRef] [Google Scholar]
- Multiple iridociliary cysts: One entity with various clinical presentations. Am J Ophthalmol Case Rep. 2022;28:101694.
- [CrossRef] [Google Scholar]
- Iris cysts: A comprehensive review on diagnosis and treatment. Surv Ophthalmol. 2018;63:347-64.
- [CrossRef] [Google Scholar]
- Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology. 1999;106:2131-5.
- [CrossRef] [Google Scholar]
- Width and pigmentation of the angle of the anterior chamber. AMA Arch Ophthalmol. 1957;58:510.
- [CrossRef] [Google Scholar]
- Anterior chamber angle assessment techniques: A review. J Clin Med. 2020;9:3814.
- [CrossRef] [Google Scholar]
- Case-based approach to managing angle closure glaucoma with anterior segment imaging. Can J Ophthalmol. 2014;49:512-8.
- [CrossRef] [Google Scholar]
- Glaucoma due to ciliary body cysts and pseudoplateau iris: A systematic review of the literature. Arq Bras Oftalmol. 2018;81:254-61.
- [CrossRef] [Google Scholar]
- An overview of treatment methods for primary angle closure. Semin Ophthalmol. 2017;32:82-5.
- [CrossRef] [Google Scholar]
- Long-term follow-up of 14 eyes with bilateral and multiple ciliary body cysts: Prognosis of this rare entity. J Glaucoma. 2021;30:e13-7.
- [CrossRef] [Google Scholar]
- medical management of glaucoma and ocular hypertension In: 2022-2023 Basic and clinical science course, section 10: Glaucoma. San Francisco: American Academy of Ophthalmology; 2022. p. :221-33. Ch. 12
- [Google Scholar]
- Long-term outcomes after acute primary angle closure in a White Caucasian population. BMC Ophthalmol. 2015;15:108.
- [CrossRef] [Google Scholar]
- Phacoemulsification for cataract extraction In: 2022-2023 Basic and clinical science course. San Francisco: American Academy of Ophthalmology; 2022. p. :138-9. Ch. 8
- [Google Scholar]







