Translate this page into:
A clinical study of the neodymium-doped yttrium–aluminium–garnet laser posterior capsulotomy: Visual outcome and early complications
*Corresponding author: Shifa Shafi Waghu, Department of Ophthalmology, Jamia Islamia Isha’atul Uloom’s Indian Institute of Medical Science and Research and Noor Hospital Badnapur, Jalna, Maharashtra, India. shifawaghu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Waghu SS, Wade BN, Ghorpade PS. A clinical study of the neodymium-doped yttrium–aluminium–garnet laser posterior capsulotomy: Visual outcome and early complications. Glob J Cataract Surg Res Ophthalmol. 2024;3:66-70. doi: 10.25259/GJCSRO_18_2024
Abstract
Objectives:
The objectives of this study were as follows: To study the efficacy of neodymium-doped yttrium–aluminium–garnet (Nd:YAG) laser capsulotomy in posterior capsular opacification (PCO) by analysing the visual outcome. To study any other early complications seen following Nd:YAG laser capsulotomy.
Materials and Methods:
A prospective interventional study was done in the Department of Ophthalmology of a tertiary care hospital in the Marathwada region of Maharashtra. A total of 55 eyes developing PCO after cataract surgery were included in the study from November 2022 to October 2023. Routine pre-laser evaluation using slit-lamp biomicroscopy, intraocular pressure (IOP) measurements and dilated fundus examination was done. Thirty-eight patients had undergone manual small incision cataract surgery with polymethyl methacrylate intraocular lens (IOL) implantation and 17 patients had undergone phacoemulsification surgery with acrylic foldable IOL implantation. The patient was then followed up on Days 2, 7, 30, and 3 months to look for any early post-laser complications.
Results:
A total of 55 eyes were included in the study. The age group of patients included in the study is from 50 to 75 years. Most of the patients 21 were in the age group of 56–60 years. Twenty (36%) were male and 35(63%) females; thus, female preponderance is seen. On retro-illumination of the slit lamp, 9 (16.3%) patients had severe PCO having vision ≤3/60, 24 (43.6%) patients had moderate PCO with vision 3/60–6/60 and 22 (40%) patients had mild PCO with vision 6/60–6/18. Forty-seven patients (85%) had visual acuity of more than 6/12 at the end of 3 months. In most patients, an appropriate central capsulotomy was achieved within the total energy of 60 mJ but in three cases more than 100 mJ energy was used due to the thick posterior capsule. About 6% of subjects showed increased IOP of more than 21 mm Hg but returned to normal level within 1 week. Mild uveal reaction in the form of anterior chamber flare and cells was seen in 2% of cases. IOL pitting was seen in 5 (8%) cases. One (2%) patient had a vision of 3/60 and a significant increase in macular thickness at day 7 post-laser which decreased at 1 month follow-up by appropriate treatment. No evidence of any retinal tears or retinal detachment seen.
Conclusion:
PCO is a common delayed complication seen after cataract surgery. This opacification decreases the vision of the patient to affect day-to-day activities. It can be easily managed on an outdoor basis by a non-invasive and effective Nd:YAG laser posterior capsulotomy procedure. This procedure has been shown to increase the visual outcome and has fewer complications which can be managed easily.
Keywords
Cataract surgery
Posterior capsule opacification
Neodymium-doped yttrium–aluminium–garnet laser
Complications
INTRODUCTION
Cataract is the most common cause of curable blindness in the world.[1] Posterior capsular opacification (PCO) or ‘secondary cataract’ is a common delayed complication seen after cataract surgery[2,3] and has a prevalence of about 50% in 5 years following cataract surgery.[4] PCO causes a decrease in visual acuity, glare, decreased contrast sensitivity, and monocular diplopia which hampers day-to-day activities and requires treatment.[5] The duration from cataract surgery to developing visually significant opacification varies from months to years and the rate of opacification declines with increasing age. PCO is formed by active lens epithelial cell proliferation, the transformation of lens epithelial cells into fibroblasts, and collagen deposition.[6] Figure 1a and 1b shows the contraction caused by myofibroblasts of epithelial cells and collagen deposition causes white fibrotic opacities hampering vision.[7] Neodymium-doped yttrium– aluminium–garnet (Nd:YAG) laser therapy is a non-invasive, effective, relatively safe technique to manage intact posterior capsules that opacify postoperatively. The use of Nd:YAG laser in the management of PCO has become easier as it has a success rate of more than 95%.[8] Laser capsulotomy was first introduced by Dr. Aron-Rosa et al.[9] and Bath and Fankhauser.[10] It uses a quick-pulsed Nd:YAG laser by applying a series of focal laser ablation shots on the posterior capsule to create a small circular opening in the visual axis as seen in Figure 1c.[11] The actual gain in visual function and improvement in the quality of life following Nd:YAG laser posterior capsulotomy in pseudophakic patients with PCO can be assessed in terms of improvement in the visual function index.[12]
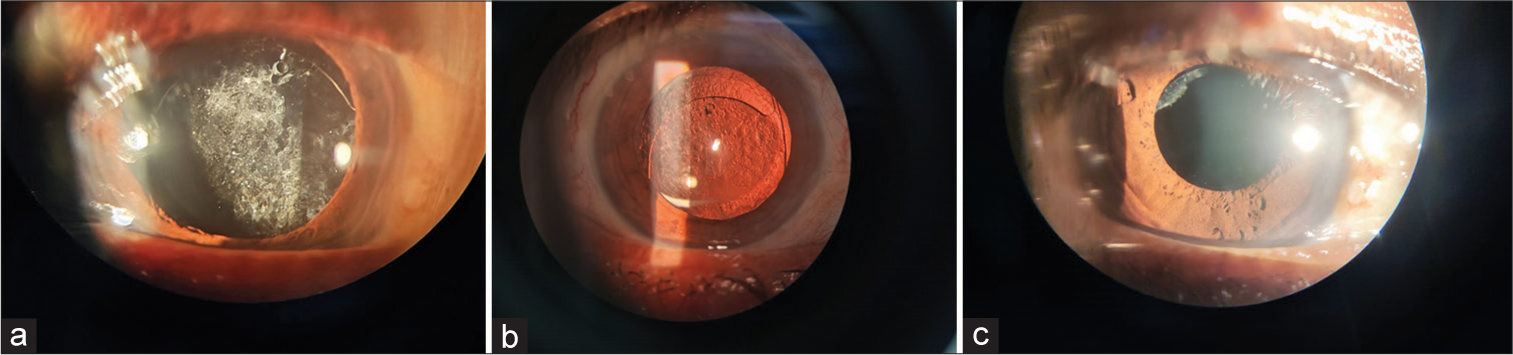
- (a) Posterior capsular opacification seen after cataract surgery. (b) Elschnig pearls seen on retroillumination of slit-lamp. (c) Post-neodymium-doped yttrium–aluminium–garnet laser posterior capsulotomy.
MATERIALS AND METHODS
A prospective interventional study was done in the Department of Ophthalmology of a tertiary care hospital in the Marathwada region of Maharashtra. Those patients satisfying the inclusion and exclusion criteria were included in the study. A total of 55 eyes were studied. The duration of the study was from November 2022 to October 2023. Only those patients attending the outpatient department (OPD) with PCO following cataract surgery for senile cataracts were included in the study. As the patients included in the study were routine OPD patients, pre-operative data regarding the type and grade of cataracts were not available. The data regarding the type of cataract surgery done and intraocular lens (IOL) implanted as obtained on pre-laser evaluation was noted. Thirty-eight patients had undergone manual small incision cataract surgery with polymethyl methacrylate IOL implantation and 17 patients had undergone phacoemulsification surgery with acrylic foldable IOL implantation. All patients had IOL placed in the bag. Exclusion criteria included patients having aphakia with PCO, any associated retinal or corneal pathologies or patients with a history of iridocyclitis, patients having dislocated IOL, patients having cortical blindness, history of trauma to the operated eye, patients having any other form of cataract like congenital cataract, developmental cataract, traumatic cataract, patients presenting within 3 months of cataract surgery, patients unable to maintain a straight posture or having psychiatric illness and any patient who is not willing to give consent. All patients were informed and explained about the procedure and written informed consent was taken. All patients underwent a complete ocular examination on all visits including visual acuity, refraction using autorefractometry (Appasamy Associates, Chennai, Tamil Nadu, India), slit-lamp biomicroscopy (Appasamy Associates, Chennai, Tamil Nadu, India) for anterior segment examination, intraocular pressure (IOP) measurement by Goldmann’s Applanation Tonometer (Appasamy Associates, Chennai, Tamil Nadu, India) and posterior segment examination by Indirect Ophthalmoscope (Appasamy Associates, Chennai, Tamil Nadu, India). The pupil was adequately dilated before the procedure with Itrop plus 0.8% tropicamide and 5% phenylephrine (Cipla, Ahmedabad, India) eye drop 3 times at 10 min intervals B/E (in both eyes). The procedure of laser capsulotomy was done by the same surgeon. The patient fixes at the red light with the other eye (non-operating). The slit lamp is focused and the Nd:YAG machine (Appasamy Associates, Chennai, Tamil Nadu, India) is switched on. The posterior capsulotomies are done by Nd:YAG laser using single pulse mode starting with 1 mJ/pulse and gradually increasing until the desired central capsulotomy size is obtained. Capsulotomy was done at 12 o’clock and then along the periphery at 3 o’clock, and 6 o’clock until the flap fall shots were applied. The energy and number of shots were recorded. Post-laser visual activity is recorded for both distant and near vision, IOP is recorded and patients were examined for complications of anterior and posterior segment. Prophylactic post-laser steroid eye drops Lotepred eye drop Loteprednol etabonate 0.2% (Sun Pharma, Nagpur, Maharashtra, India) given to the patient 4 times a day for 1 week. No anti-glaucoma drops were given to the patient before or after the procedure. Patients were followed up on days 2, day 7, 30, and 3 months for early complications. Optical coherence tomography (Appasamy Associates, Chennai, Tamil Nadu, India) was used to confirm cystoid macular edema post-laser in patients whose macula showed elevation on indirect ophthalmoscopy.
RESULTS
A total of 55 eyes 20 males and 35 females were included in the study. The right eye was affected in 25 cases and the left eye was affected in 30 cases.
The age group of patients included in the study is from 50 years to 75 years. The grading of PCO was done according to the evaluation of PCO grading which is a morphological scoring system based on examining the PCO on retro-illumination of slit lamp.[13,14] Nine (16.3%) patients had severe PCO having vision ≤3/60, 24 (43.6%) patients had moderate PCO with vision 3/60–6/60, and 22 (40%) patients had mild PCO with vision 6/60–6/18 [Table 1]. The post-laser visual acuity at 3 months increased to 47 (85.45%) patients having a visual acuity of ≥6/18 and 8 (14.54%) patients having a visual acuity of 6/60–6/18 [Table 2]. The total energy used for capsulotomy was calculated by taking into account the power and number of shots applied and ranged from 11 mJ to 120 mJ. In most cases, the desired response was obtained within the total energy of 60 mJ but in three cases, more than 100 mJ energy was used due to the thick posterior capsule [Table 3]. Please refer to Tables and Graphs for results.
| Grade of PCO | Visual Acuity | Number of patients |
|---|---|---|
| Grade 4 (severe) | </=3/60 | 9 (16.3%) |
| Grade 3 (moderate) | 3/60-6/60 | 24 (43.6%) |
| Grade 2 (mild) | 6/60-6/18 | 22 (40%) |
| Grade 1 (minimal) | >/=6/18 | 0 |
PCO: Posterior capsular opacification
| Visual Acuity | Pre-Laser | Post-Laser | |||
|---|---|---|---|---|---|
| Day 2 | Day 7 | Day 30 | 3 months | ||
| </=3/60 | 9 | 0 | 0 | 0 | 0 |
| 3/60-6/60 | 24 | 3 | 1 | 1 | 0 |
| 6/60-6/18 | 22 | 18 | 14 | 9 | 8 |
| >/=6/18 | 0 | 34 | 40 | 46 | 47 |
| Total Energy (mJ) | Number of eyes | % |
|---|---|---|
| <20 | 9 | 16.3% |
| 21-40 | 18 | 32.7% |
| 41-60 | 11 | 20% |
| 61-80 | 10 | 18.1% |
| 81-100 | 4 | 7.2% |
| >100 | 3 | 5.4% |
DISCUSSION
A total of 55 eyes were included in the study. The age group of patients included in the study is from 50 to 75 years. Most of the patients 21 (38%) were in the age group of 56–60 years. Twenty (36%) were male and 35 (63%) females; thus, female preponderance is seen. The study done by Tayyab et al.[15] had male preponderance but a study by Sarkar et al.[16] shows female preponderance. The interval between cataract surgery and the development of PCO in our study ranged from 6 months to 6.5 years (Mean = 2.16 ± 1.28 years). The study by Parajuli et al. had a mean duration of 3.26 ± 1.74 years in Group 1 and 2.46 ± 1.37 years in Group 2.[17] In our study, 19 (35%) patients developed PCO 1–2 years after cataract surgery followed by 15 (27%) patients who developed PCO within 6 months-1 year after cataract surgery [Table 4]. The study by Das et al.[18] shows a 6-month mean period for the development of PCO after cataract surgery. In our study, the Elschnig pearl type of PCO was seen commonly compared to the fibrous type which was also noted by Soujanya and Kanthamani[19] The incidence of developing posterior capsule opacification was comparatively less with acrylic hydrophilic IOLs than with other materials like Polymethyl Methacrylate (PMMA) as seen in the study by Hayashi et al.[20] and also observed in our study. Jain et al.[21] reported an improvement in visual acuity by Snellen’s vision chart in 90.7% of cases. Significant visual improvement was seen in 98% of cases in the study by Sirisha and Chowdary.[22] In our study at day 2, 34 (61%) patients had visual acuity improvement of 6/12–6/6 which increased to 47 (85%) at the end of 3 months. Eight (14%) patients had visual acuity of 6/60–6/18 at the end of 3 months. One (2%) patient had a vision of 3/60 and a significant increase in macular thickness at day 7 post-laser as a result of using high energy. Ari et al.[23] observed a significant increase in macular thickness following Nd:YAG capsulotomy in patients receiving high energy. Karahan et al.[24] found a significant increment in central macular thickness after Nd:YAG capsulotomy at 1 week which decreased to pre-operative levels at 4 weeks irrespective of the capsulotomy size. In our study also, the macular thickness decreased to pre-laser levels at 1-month follow-up using 0.5% ketorolac eye drops [Table 5]. In the absence of antiglaucoma or anti-inflammatory prophylaxis, 59–67% of patients showed IOP increment of at least 10 mm Hg following Nd:YAG laser capsulotomy.[25] Ozkurt et al.[26] concluded no significant change in IOP after Nd:YAG capsulotomy. Raised IOP occurred in 2.8% in the study by Sirisha and Chowdary.[22] However, in our study, 6% of subjects showed increased IOP of more than 21 mm Hg but returned to normal level within 1 week after using Iotim eye drops 0.5% timolol maleate (Pixel, Waluj, Maharashtra, India) [Table 6]. The most likely mechanism for this transient pressure elevation is blockage of trabecular meshwork by cortical and capsular debris. A transient rise of post-laser IOP 10 mmHg was found in 5% of cases. In our study, IOL pitting was seen in 5 (8%) cases; however, this did not cause any disturbance in visual acuity [Table 5]. Jain et al.[21] and Naseem et al.[27] reported IOL pitting in 2% and 4% cases, respectively. Shah et al.[28] reported 0.1% of subjects having post-laser uveitis. Mild anterior chamber reaction in the form of iritis was seen in 10% of cases at post-laser day 1 in the study by Das et al.[18] In our study, we noted anterior chamber flare and cells in 1 (2%) case which was managed by giving low-dose steroid eye drops for 1 week [Table 5]. No case developed any retinal tear or retinal detachment.
| Time Interval | Number of cases | Percentage |
|---|---|---|
| 0-6 months | 3 | 5% |
| 6 months – 1 year | 15 | 27% |
| 1 – 2 years | 19 | 35% |
| 2-3 years | 9 | 16% |
| 3-4 years | 6 | 11% |
| 4-5 years | 2 | 4% |
| 5-6 years | 0 | 0.00% |
| 6-7 years | 1 | 2% |
| Total | 55 | 100% |
| Complication | Number of cases | Percentage |
|---|---|---|
| IOL pitting | 5 | 8% |
| Transient raised IOP | 4 | 6% |
| Uveal reaction | 1 | 2% |
| Cystoid macular edema (CME) | 1 | 2% |
IOP: Intraocular pressure, IOL: Intraocular lens
| IOP Measurement | Pre-Laser | Post-Laser | |||
|---|---|---|---|---|---|
| Day 2 | Day 7 | Day 30 | 3 months | ||
| 0-10 | 8 | 6 | 7 | 8 | 8 |
| 11-20 | 47 | 45 | 48 | 47 | 47 |
| >21 | 0 | 4 | 0 | 0 | 0 |
IOP: Intraocular pressure
CONCLUSION
Intracapsular cataract extraction surgery was a commonly done cataract surgery in the past. However, nowadays, the surgery of choice is extracapsular cataract extraction with intraocular lens implantation. PCO is a common delayed complication seen after cataract surgery. Initially, the opening of the posterior capsule was done by invasive surgical means which caused serious posterior segment complications such as cystoid macular edema, retinal tears, and retinal detachment. After the advent of the Nd:YAG laser, posterior capsule openings can be made non-invasively as an outdoor procedure and it provides excellent posterior capsulotomies. From our study, it is evident that Nd:YAG laser posterior capsulotomy is a safe and effective procedure for capsulotomy. The post-operative visual acuity results are very good and the early complication rate is low which can be easily managed.
Acknowledgment
I would like to thank my HOD Dr. Rupali Rangu for allowing me to do this research in my department and also thanks to all my teachers who helped me throughout my research.
Ethical approval
The research/study was approved by the Institutional Review Board at JIIU’s Indian Institute of Medical Science and Research, number IIMSR/IEC/PG/2022/03, dated October 7, 2022.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- The prevalence of lens opacities in Tehran: The Tehran Eye Study. Ophthalmic Epidemiol. 2009;16:187-92.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior capsule opacification In: Kohnen T, Koch DD, eds. Ophthalmology (4th ed). New York: Elsevier; 2014. p. :407-11.
- [Google Scholar]
- A randomized controlled trial of peeling and aspiration of Elschnig pearls and neodymium: Yttrium-aluminium-garnet laser capsulotomy. Int J Ophthalmol. 2015;8:590-6.
- [Google Scholar]
- 5 year incidence of YAG capsulotomy and PCO after cataract surgery with single-piece monofocal intraocular lenses: A real-world evidence study of 20,763 eyes. Eye (Lond). 2020;34:960-8.
- [CrossRef] [PubMed] [Google Scholar]
- Natural course of elschnig pearl formation and disappearance. Invest Ophthalmol Vis Sci. 2010;51:1547-53.
- [CrossRef] [PubMed] [Google Scholar]
- Histological comparison of in vitro and in vivo development of peripheral posterior capsule opacification in human donor tissue. Exp Eye Res. 2019;188:107807.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior capsule opacification: A cell biological perspective. Exp Eye Res. 2002;74:337-47.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior capsule opacification: A review of the aetiopathogenesis, experimental and clinical studies and factors for prevention. Indian J Ophthalmol. 2004;52:99-112.
- [Google Scholar]
- Use of the neodymium-YAG laser to open the posterior capsule after lens implant surgery: A preliminary report. J Am Intraocul Implant Soc. 1980;6:352-4.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term results of Nd:YAG laser posterior capsulotomy with the Swiss laser. J Cataract Refract Surg. 1986;12:150-3.
- [CrossRef] [PubMed] [Google Scholar]
- A new technique for Nd:YAG laser posterior capsulotomy. Int J Ophthalmol. 2014;7:345-9.
- [Google Scholar]
- Visual function and quality of life in pseudophakic patients before and after capsulotomy. Eur J Ophthalmol. 2012;22:943-9.
- [CrossRef] [PubMed] [Google Scholar]
- Photographic image analysis system of posterior capsule opacification. J Cataract Refract Surg. 1997;23:1515-20.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of posterior subcapsular opacification on vision and visual function among subjects undergoing cataract surgery in rural China: Study of Cataract Outcomes and Up-Take of Services (SCOUTS) in the Caring is Hip Project, Report 5. Brit J Ophthalmol. 2008;92:598-603.
- [CrossRef] [PubMed] [Google Scholar]
- Frequency of posterior capsular opacification following PMMA vs. slicon posterior chamber IOL implantation with phacoemulsification. Pak J Ophhalmol. 2004;20:96-9.
- [Google Scholar]
- Visual outcome following Nd:YAG laser capsulotomy in posterior capsularopacification in pseudophakic adult patients-a prospective observational study in atertiary care centre. Indian J Clin Exp Ophthalmol. 2020;6:343-6.
- [CrossRef] [Google Scholar]
- Effect of Nd:YAG laser posterior capsulotomy on intraocular pressure, refraction, anterior chamber depth, and macular thickness. Clin Ophthalmol. 2019;13:945-52.
- [CrossRef] [PubMed] [Google Scholar]
- Effects of neodymium-doped yttrium aluminium garnet (Nd:YAG) laser capsulotomy on visual outcomes from a lower-middle income country. Cureus. 2021;13:e17895.
- [CrossRef] [Google Scholar]
- Visual outcomes and complications after Neodymium-doped yttrium aluminium garnet laser capsulotomy in Posterior capsular opacification. Indian J Clin Exp Ophthalmol. 2019;5:491-5.
- [CrossRef] [Google Scholar]
- Long-term effect of surface light scattering and glistenings of intraocular lenses on visual function. Am J Ophthalmol. 2012;154:240-51.e2.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of Nd:YAG laser capsulotomy in pseudophakic eyes with special reference to iop changes. J Evol Med Dent Sci. 2014;3:12627-35.
- [CrossRef] [Google Scholar]
- Visual outcome of Nd-YAG laser capsulotomy in posterior capsule opacification. J Evol Med Dent Sci. 2016;5:1479-82.
- [CrossRef] [Google Scholar]
- The effects of Nd:YAG laser posterior capsulotomy on macular thickness, intraocular pressure, and visual acuity. Ophthalmic Surg Lasers Imaging Retina. 2012;43:395-400.
- [CrossRef] [PubMed] [Google Scholar]
- The effect of ND: YAG laser posterior capsulotomy size on refraction, intraocular pressure, and macular thickness. J Ophthalmol. 2014;2014:846385.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant glaucoma as a complication of Nd:YAG laser posterior capsulotomy. Ophthalmic Surg Lasers Imaging. 2004;35:248-50.
- [CrossRef] [PubMed] [Google Scholar]
- Refraction, intraocular pressure and anterior chamber depth changes after Nd:YAG laser treatment for posterior capsular opacification in pseudophakic eyes. Clin Exp Optometry. 2009;92:412-5.
- [CrossRef] [PubMed] [Google Scholar]
- Visual outcome and complications after Nd:YAG laser capsulotomy in patients with posterior capsular opacification. Pak J Med Res. 2010;49:22-4.
- [Google Scholar]
- Three thousand YAG lasers in posterior capsulotomies: An analysis of complications. Ophthalmic Surg. 1986;17:473-7.
- [CrossRef] [Google Scholar]






