Translate this page into:
Bilateral spontaneous late anterior dislocation of in-the-bag intraocular lens with phimosis in uveitis patient
*Corresponding author: Vinita Ramnani, Department of Ophthalmology, Bansal Hospital, Bhopal, Madhya Pradesh, India. ramnanivinita@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Ramnani V, Ramnani S. Bilateral spontaneous late anterior dislocation of in-the-bag intraocular lens with phimosis in uveitis patient. Glob J Cataract Surg Res Ophthalmol. doi: 10.25259/GJCSRO_3_2024
Abstract
The late in-the-bag dislocation of the intraocular lens (IOL) is an uncommon complication in uveitis patients and can occur after uneventful surgery as a result of progressive zonular dehiscence. A 57-year-old diabetic and uveitic male developed bilateral spontaneous anterior dislocation of in-the-bag IOLs with phimosis following 15 and 23 months, respectively, in the right and left eye after uneventful phacoemulsification with foldable IOL. The dislocated bag and IOL complex were removed and scleral fixated IOL (SFIOL) was implanted in both eyes with good results. Late in-the-bag dislocation of IOL could be multifactorial, and its management is challenging. Many surgical options are available to handle such situations, but dislocated IOL replacement with SFIOL is a good option for restoring and maintaining the vision of such eyes.
Keywords
Late in-the-bag dislocation
Scleral fixated intraocular lens
Uveitis
Phimosis
INTRODUCTION
Phacoemulsification with an in-the-bag foldable intraocular lens (IOL) with good inflammatory control is standard treatment in uveitis with cataracts. However, complications such as secondary glaucoma, recurrence of uveitis, anterior or posterior capsule opacification, phimosis, subluxation or dislocation of IOL, and cystoid macular oedema can occur after uneventful cataract surgery in uveitic cataract. The incidence of posterior chamber IOL decentration or dislocation varies between 0.2% and 3%.[1] Spontaneous bilateral anterior inthe-bag IOL dislocation is extremely rare.[2] Reporting a case of spontaneous bilateral anterior in-the-bag IOL dislocation with phimosis in a uveitis patient occurred 15 and 23 months following uneventful cataract surgery and its successful management. Posterior dislocation of the IOL bag complex is more common than anterior dislocation. This case report highlights rare presentations, although management of such cases remains standard. This presentation aims to make clinicians aware of this entity, especially in high-risk patients, so that these consequences can be well anticipated and by proper care complications of phimosis are obviated.
CASE REPORT
A 57-year-old male diabetic patient with bilateral recurrent uveitis of unknown aetiology underwent uneventful phacoemulsification with foldable IOL in both eyes for visually significant posterior subcapsular cataract. Postoperatively, the patient was doing well with the best corrected visual acuity 6/12-N/9 in the right eye (RE) and 6/9-N/9 in the left eye (LE) on regular follow-up and treatment. Six months following surgery presented with black floaters and difficulty in reading and driving in both eyes. On examination, a dense fibrosis of the anterior capsule with shrinkage to phimosis and a slight upwards shift of the IOL capsular bag complex with excessive movement in RE was seen [Figure 1a]. LE showed a thickened anterior capsule with sufficient central capsular opening and mild subluxation [Figure 1b]. After control of inflammation and secondary glaucoma, the vision improved to 6/18 RE and 6/12 LE. The patient continued with satisfactory vision on medical treatment and follow-up for nearly 6 months showed no further progression of subluxation. Unfortunately, 15 months following surgery, the patient reported with sudden marked reduction of vision in RE to hand movement. Slit-lamp examination showed anterior dislocation of the bag IOL complex [Figure 1c]. The IOL bag complex was removed and SFIOL was implanted in RE with best corrected visual acuity of 6/12 after 1 month [Figure 1d]. The patient received a routine post-operative treatment regimen of antibiotic eye drops for a week and tapering dosage of steroids for 6 weeks and non-steroidal anti-inflammatory for 8 weeks. Nearly 8 months following RE surgery, a similar episode occurred in LE with a marked reduction of vision to the count finger. The LE showed spontaneous late dislocation of the bag IOL complex in the anterior chamber [Figure 1e] and a similar procedure was adopted for LE also, following which the patient regained 6/9 vision [Figure 1f]. Postoperatively, both eyes were quiet, IOP was 16 mmHg by applanation tonometer and refraction of +1.50 DC × 180° in RE and + 1.00 DS +1.50 DC× 180° in LE with near correction of +2.75 Dsph N/9 at 24-month follow-up.
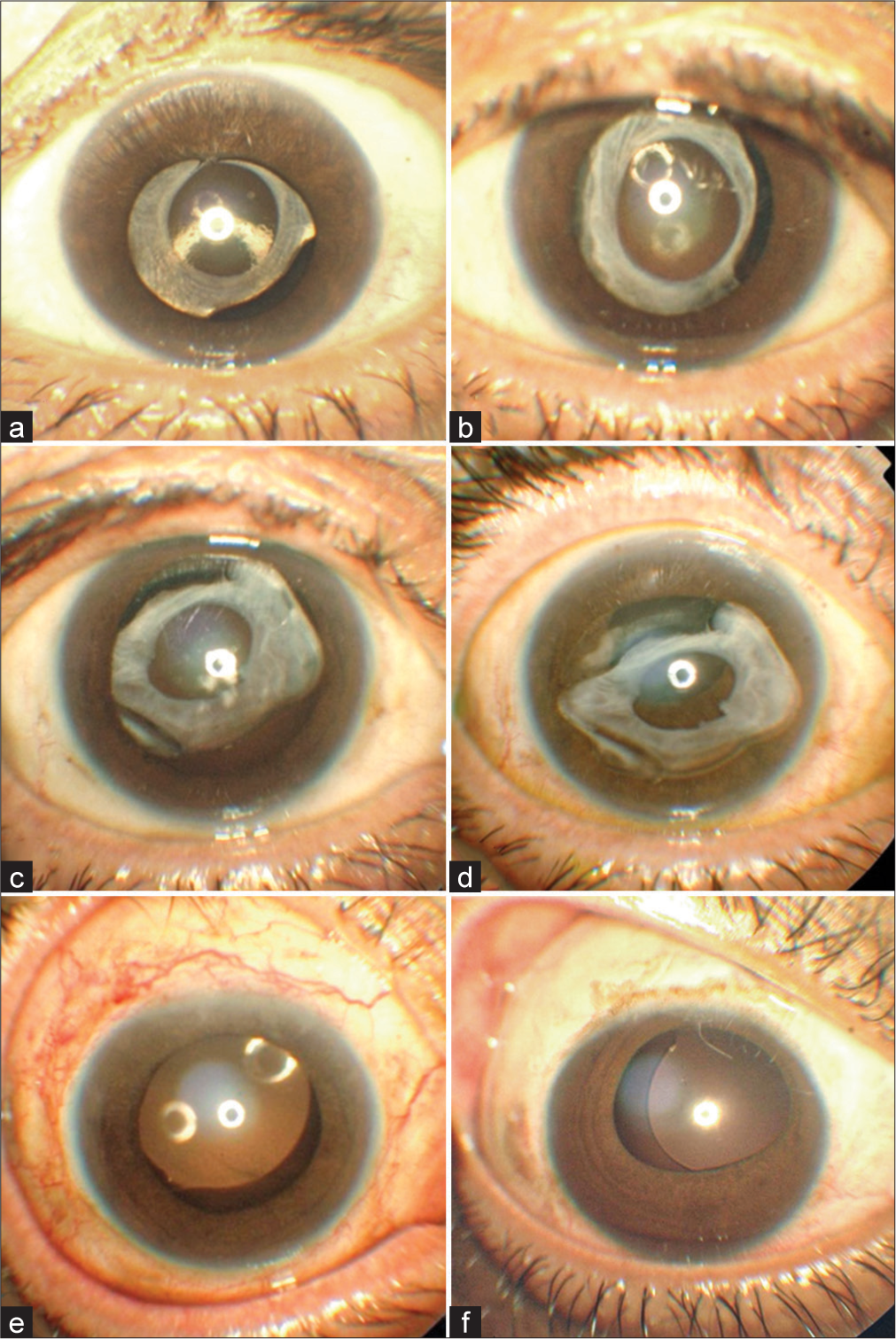
- (a) RE – 6 months following surgery RE dense fibrosis of anterior capsule with shrinkage to phimosis and slight upwards shift of IOL capsular bag complex. (b) LE – thickened anterior capsule with sufficient central capsular opening and mild subluxation. (c) RE – anterior dislocation of bag IOL complex. (d) LE – anterior dislocation of bag IOL complex. (e) RE SFIOL. (f) LE SFIOL. RE: Right eye, LE: Left eye, IOL: Intraocular lens, SFIOL: Scleral fixated intraocular lens.
DISCUSSION
The pre-operative risk factors for IOL decentration and phimosis could be pseudoexfoliation, uveitis, myopia, vitrectomy, and trauma.[3] Intraoperative zonular dehiscence, post-operative anterior capsular contraction syndrome, and trauma are common risk factors for IOL decentration or dislocation. The early IOL dislocation occurs mainly because of poor IOL fixation, either due to loss of capsular or zonular integrity or asymmetric placement of the haptics during surgery. The late dislocation of IOL may occur anytime from 1 month to 8½ years following surgery.[4] In patients with uveitis, intracapsular dislocation of the crystalline lens has been reported.[5] There can be chances of zonular instability due to the extension of inflammation to pars plicata, and an altered blood-aqueous barrier may lead to epithelial cell proliferation and increased risk of capsule contraction. In our case, there was anterior capsular contraction and phimosis, which increased the subluxation of the bag. Besides this, a small diameter capsulorhexis is commonly associated with phimosis, and primary prevention for phimosis includes a larger capsulorhexis size, meticulous lens epithelial cells cleanup during phacoemulsification[6], or anterior capsule Nd: YAG relaxing incisions soon after phacoemulsification[7] in high-risk patients.
The management of dislocated IOL in uveitic eyes can be very challenging. Conservative management is helpful in difficult uveitis patients or those with tolerable symptoms. Surgical options would be either fixation of the existing IOL or removal of the dislocated IOL and insertion of another IOL such as anterior chamber IOL (ACIOL), iris fixated IOL (IFIOL) and posterior chamber IOL (PCIOL) SFIOL either sutured or glued. Choice of surgical option depends on type of case and individual surgeon preference. In a study by Steeples and Jones of 1056 uveitis patients, only 6 (0.57%) developed IOL dislocation and found that angle-supported or iris-enclaved IOLs were not safe and scleral fixated PCIOLs were favoured approach. ACIOLs in uveitic eyes can lead to exacerbations and recurrences of uveitis leading to vision-threatening complications therefore not considered a good option.[8] A case series of five late in-thebag IOL dislocations in uveitis (mean displacement time of 81 months) showed good outcomes by lens explantation and replacement with ACIOL.[9] The study showed that ACIOL can still be an important option in uveitic patients.[10] At present, the decision of type of lens ACIOL or iris or scleral sutured PCIOL in uveitic IOL dislocation is controversial. Bilateral dislocation of in-the-bag IOLs into the vitreous cavity after 24 and 41 months following cataract surgery in a patient with intermediate uveitis was managed effectively by pars plana vitrectomy and sutured PCIOL.[11] The preferred method of management of a dislocated IOL in uveitic eyes is pars plana vitrectomy with IOL refixation within the bag or IOL removal and pars plana scleral fixated IOL, as shown in the study of 581 eyes of uveitis patients with 11 (1.89%) late in-the-bag IOL dislocation.[12] Overall management of in-the-bag IOL dislocation requires special considerations; surgical options are many, and in literature, the indications, optimal timing and type of surgery for management have not been clearly established. However, there is a definite advantage of SFIOL over ACIOL and IFIOL with regard to complications such as chronic recurrent uveitis, corneal endothelial damage, and raised IOP. In our case, uveitis, diabetes, and capsular contraction together were responsible for spontaneous dislocation of the IOL, and management by IOL exchange with limited anterior vitrectomy and SFIOL was found to be a safe and effective option.
CONCLUSION
Late in-the-bag dislocation of IOL is a known complication in uveitic eyes, but rare causes may be multifactorial, and management of such cases is a challenge. Surgical management of IOL replacement with SFIOL is a good option for restoring and maintaining vision for such eyes.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Outcome of phacoemulsification in patients with uveitis. Br J Ophthalmol. 2007;91:916-21.
- [CrossRef] [PubMed] [Google Scholar]
- Late in-the-bag spontaneous intraocular lens dislocation: Evaluation of 86 consecutive cases. Ophthalmology. 2009;116:664-70.
- [CrossRef] [PubMed] [Google Scholar]
- Late in the bag intraocular lens dislocation: Incidence, prevention, and management. J Cataract Refract Surg. 2005;31:2193-204.
- [CrossRef] [PubMed] [Google Scholar]
- Late in-the-bag intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Acta Ophthalmol. 2014;92:184-91.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous lens subluxation in uveitis. Am J Ophthalmol. 1990;110:714-6.
- [CrossRef] [PubMed] [Google Scholar]
- Removal of lens epithelial cells and the effect on capsulorhexis size. J Cataract Refract Surg. 2005;31:1569-74.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior capsule relaxing incisions with neodymium: YAG laser for patients at high-risk for anterior capsule contraction. J Cataract Refract Surg. 2011;37:97-103.
- [CrossRef] [PubMed] [Google Scholar]
- Late in the bag intraocular lens dislocation in patients with uveitis. Br J Ophthalmol. 2015;99:1206-10.
- [CrossRef] [PubMed] [Google Scholar]
- In bag dislocation of intraocular lens in patients with uveitis: A case series. J Ophthalmic Inflamm Infect. 2015;5:10.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior chamber intraocular lens implantation in patients with a history of chronic uveitis: Five year follow up. J Cataract Refract Surg. 2014;40:77-81.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral dislocation of in the bag posterior chamber intraocular lenses in a patient with intermediate uveitis. J Cataract Refract Surg. 2003;29:2013-4.
- [CrossRef] [PubMed] [Google Scholar]
- Late dislocation of in-the-bag intraocular lenses in uveitic eyes: An analysis of management and complications. Indian J Ophthalmol. 2017;65:148-54.
- [CrossRef] [PubMed] [Google Scholar]






