Translate this page into:
Hypoparathyroidism: A dark horse differential in young age cataracts
*Corresponding author: Mayur R. Moreker, Department of Ophthalmology, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India. eyeinflammation@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Thakre NM, Moreker MR, Mehta N, Desai M, Jaggi S, Mehta S. Hypoparathyroidism: A dark horse differential in young age cataracts. Glob J Cataract Surg Res Ophthalmol. 2024;3:75-8. doi: 10.25259/GJCSRO_14_2024
Abstract
In India, cataracts account for the lion’s share of cases of blindness. Age is still the single most important risk factor for cataracts. Cataracts in the young adult age group are less common and are usually secondary to various local and systemic conditions. The aetiology may be a challenging one to ascertain in certain cases of young-age cataracts. A rapidly developing cataract in a young age individual may further add to the diagnostic dilemma especially when the patient presents with multi-system affection necessitating the widening of the horizons of suspected local and systemic pathologies at play. Therefore, we report a case of a 25-year-old lady who presented with a history of seizures, headache, disc oedema and progressive bilateral blurring of vision due to rapidly developing cataracts over 4 months in a case of primary hypoparathyroidism. Correction of the underlying abnormalities resulted in the resolution of disc oedema and headache. Furthermore, the patient had no episodes of seizures in the 1½ years of follow-up. In addition, full visual recovery was achieved after bilateral cataract surgery. Awareness of this rare presentation can help in the early diagnosis and evaluation of cataracts, besides correction of the systemic pathologies for an overall better patient outcome.
Keywords
Hypoparathyroidism
Hypocalcaemia
Papilledema
Juvenile cataract
Seizure disorder
INTRODUCTION
In India, cataracts account for up to 80% of the cases of blindness. Although cataract has a multifactorial aetiology, age is still the most important risk factor for cataracts.[1] Cataracts in the young adult age group are less common and usually secondary to eye trauma, intraocular inflammation, diabetes mellitus, inborn errors of metabolism, chronic hypocalcaemia and prolonged use of steroids. Allergic dermatitis, chronic uveitis, high myopia and prolonged dehydration are also risk factors for young-age cataracts. Posterior subcapsular cataract (PSC) is the predominant type of cataract prevalent in young patients.[1] Young adult cataracts due to hypocalcaemia due to primary hypoparathyroidism are rare. Common ophthalmic involvements include papilledema and early cataracts.[2] Patients present with muscle cramps, tetany, fatigue, paraesthesia, headache and abdominal pain. Seizures and cardiac arrhythmias are life-threatening emergencies associated with hypocalcaemia. On reviewing the literature, we found various case reports of hypoparathyroidism with cataracts or basal ganglia calcification. However, there are very few reports of rapidly developing cataracts with multiple systemic manifestations and radiological features in the same patient. Most of the available literature depicts gradually progressing bilateral cataracts in patients of hypocalcaemia due to primary hypoparathyroidism over the years.
CASE REPORT
A 25-year-old thin-built (weight 39.4 kgs/Height 150 cm) lady presented with headache and blurring of vision in both eyes for 3 months. The headache was not localised to any specific area. The patient was a known case of seizure disorder with the first episode of generalised tonic-clonic seizure 7 years back. Magnetic resonance imaging of the brain done at that time was unremarkable. The patient was started on leviracetam 500 mg BD and stopped in 2019 on her own. Following this, the patient had a seizure episode and the frequency of seizures remained constant at 1–2 episodes/year. The patient was not receiving any treatment during this period. The patient also complained of episodes of anxiety and occasional tingling in the bilateral hands and feet during this period. Her vital parameters were within normal range. The neurological examination revealed a conscious and oriented patient obeying commands with a Glasgow coma scale of 15/15, and normal speech with no sensory or motor deficits. Other systemic examinations were also within normal limits. However, her computed tomography (CT) brain showed soft and hard calcification in the bilateral lentiform nucleus [Figure 1]. Lumbar puncture was performed with normal-opening pressure (145 mm H2O), and the cerebrospinal fluid (CSF) sample yielded normal results. Ophthalmic evaluation of the patient revealed visual acuity of both eyes of 20/40, N6, which improved to 20/30, N6 in the right eye and 20/20p and N6 in the left eye after refraction. Her colour vision and Amsler’s grid examination were normal; pupils were round, regularly reactive to light and bilaterally equal with diffuse PSCs in both eyes. Fundus examination revealed severe papilledema (R>L) with venular dilatation and tortuosity [Figure 2a and b]. Further, investigations revealed mild anaemia (haemoglobin 11.2 g/dL), elevated erythrocyte sedimentation rate (26 mm/h), creatine phosphokinase (2314 mIU/mL), creatine kinase-MB (7.62 ng/mL), serum glutamic-oxaloacetic transaminase (65 mU/mL), severe hypokalaemia (2.30 mEq/L), hypochloraemia (97 mEq/L), hypocalcaemia (2.90 mg%), hypovitaminosis D3 (4.8 ng/mL) and hypoparathyroidism (2.60 pg/mL). The electrocardiogram (ECG) of the patient revealed a prolonged QT interval with T-wave inversion. C-reactive protein, serum sodium and serum ceruloplasmin were within the normal range. Thus, primary hypoparathyroidism leading to hypocalcaemia was adjudged to be the causative factor for seizures, tetanic cramps and paraesthesia. The CT brain findings, ECG findings and ophthalmic findings of bilateral papilledema and cataract were consistent with hypocalcaemia. Based on this, the patient was treated with anti-epileptic and anti-anxiety medications. In addition, the patient was given Vitamin D, calcium and potassium supplementation to correct the respective deficiencies. As her investigations did not reveal any other cause for papilledema, it was considered to be due to hypocalcaemia. Thus, it was considered that correction of hypocalcaemia would lead to the resolution of papilledema. A follow-up ophthalmic examination after 1 week revealed further deterioration in visual acuity. The visual acuity in her right eye was reduced to Fc @ 1.5 Mt, N18 and in the left eye to 20/30, N6. It was seen that the right eye cataract had progressed into a mature cataract and the left eye had a PSC + Cortical Cataract. Zonular weakness was noticed in both eyes. Fundus examination revealed a very hazy view in the right eye compared to the left eye and indicated a mild reduction in disc oedema, venular tortuosity and dilatation compared to the previous examination [Figure 2c and d]. The patient underwent right eye cataract surgery (Phacoemulsification) with Posterior Chamber Intraocular Lens (PCIOL) implantation with a visual outcome of 20/40, N6. Two months later, she underwent surgery for a left eye cataract (Phacoemulsification) where the visual outcome of 20/20, N12 was attained. Binocularly, she had a visual acuity of 20/20, N6. In addition, disc oedema was significantly reduced [Figure 2e and f] with no episodes of seizures during the intervening period.

- Computed tomography brain (plain) of a 25-year-old lady presenting with headache and blurring of vision diagnosed with primary hypoparathyroidism showing calcification in the bilateral lentiform nucleus (indicated by yellow arrows).
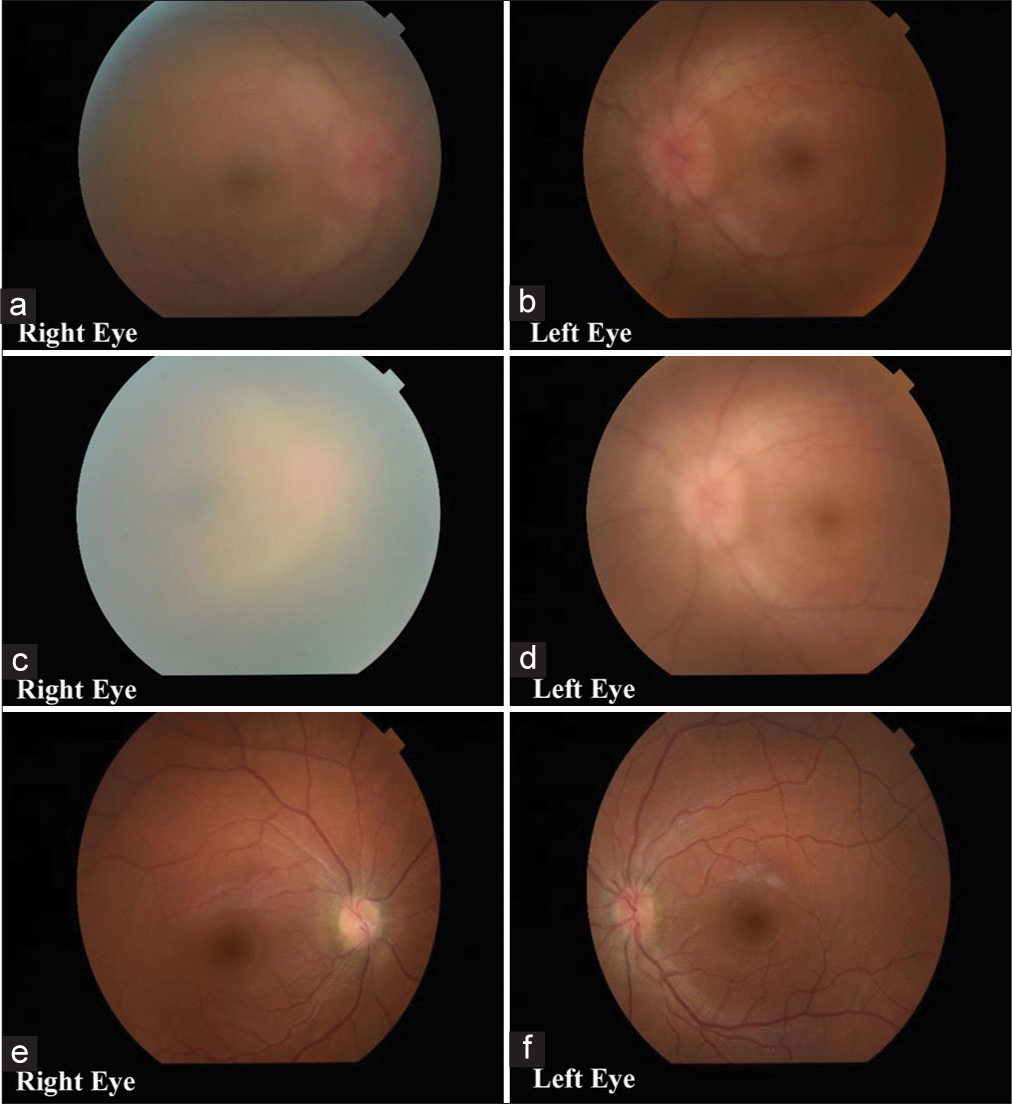
- Fundus images of a 25-year-old lady presenting with headache and blurring of vision diagnosed with primary hypoparathyroidism. (a and b) Bilateral papilledema with venular dilatation and tortuosity; Hazy fundus view due to posterior subcapsular cataract. (c and d) Right eye cataract progression. Very hazy fundus view in the right eye with a mild reduction in disc oedema; venular tortuosity and dilatation compared to the previous examination. (e and f) A clear view of the fundus after cataract surgery. Resolving disc oedema with a reduction in venous dilatation and tortuosity is seen.
DISCUSSION
Hypoparathyroidism is a rare endocrine disorder characterised by low serum calcium and parathyroid hormone levels. Parathyroid iatrogenic surgical removal is one of the common causes. However, various conditions can cause hypoparathyroidism. The severity and rate of development of hypocalcaemia determine its clinical manifestations. The clinical presentation of hypoparathyroidism varies depending on the duration of hypocalcaemia.[3] It manifests acutely as muscular cramps, tetany, paraesthesia, cardiac arrhythmias, altered mental status and seizures. Cataracts, basal ganglia calcifications, dilated cardiomyopathy, dementia and cerebellar dysfunction are chronic manifestations.[4] An occasional complication of hypoparathyroidism is extensive intracranial calcification. Prolonged hypocalcaemia and hyperphosphatemia promote the deposition of calcium-phosphorus complexes in the brain parenchymal tissue. Increased expression of osteogenesis-related molecules such as osteonectin/osteopontin in the caudate nucleus and grey matter could favour metastatic calcification in hypoparathyroidism.[5] Ophthalmic involvements include papilledema, early cataracts, corneal changes, photophobia and blepharospasm, blepharitis, lid pigmentation, strabismus and ptosis.[2] Cataract is the most common ocular symptom. Cataracts associated with idiopathic hypoparathyroidism possess characteristic manifestations, and long-standing severe hypoparathyroidism and hypocalcaemia increase the risk of cataracts. Hypocalcaemia causes bilateral lens abnormalities. It presents as punctate, iridescent opacities in the anterior and posterior cortex. These opacities are separated from the lens capsule by a clear zone, which may remain stable or mature into total cataracts as seen in our patient [Figure 3a and b]. Interference in calcium metabolism results in the deposition of insoluble calcium salts in the lens, resulting in the development of cataracts. Hypocalcaemia affects optic nerve head function. There may be Papilledema with minimal or no reduction in visual acuity with enlargement of the blind spot.[6] The CSF pressure can vary greatly from normal to values as high as 460 mm in water. Less commonly, the clinical presentation is of optic neuritis, with a marked reduction in visual acuity, abnormal colour vision and relative afferent pupil defect.[6] Multiple theories exist for explaining the mechanism of papilledema, such as increased intracranial pressure secondary to either CSF hypersecretion caused by increased choroid plexus adenylate cyclase activity[3] or decreased CSF absorption, as demonstrated by radio iodinated serum albumin cisternography.[7] However, there are case reports that show that the CSF pressures were normal, leading to the possibility of another mechanism of axonal damage. According to them, differences in CSF pressure may exist within different compartments of the subarachnoid space, with elevated local CSF pressure at the optic nerve head possibly causing ischaemic neuronal loss.[8] McLean et al. postulated that hypocalcaemia decreases axonal transport, leading to axonal and optic disc swelling. This, in turn, results in anterior ischaemic optic neuropathy. This localised effect of hypocalcaemia on optic nerve function could explain cases in which the CSF pressure is normal.[9] Optic neuropathy associated with hypocalcaemia improved following the initiation of calcium therapy. However, treatment should be initiated early to prevent optic atrophy. Surgical removal of the cataract in cases of serious visual impairment is advised.[10]
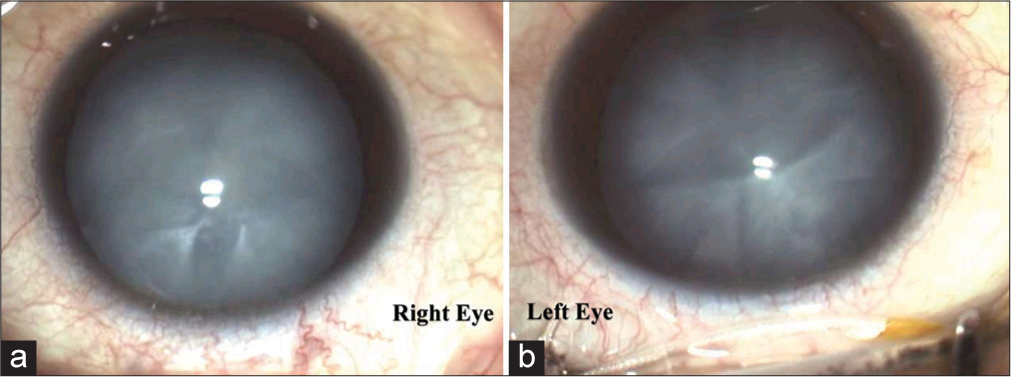
- (a and b) Ocular images of a 25-year-old lady presenting with headache and blurring of vision diagnosed with primary hypoparathyroidism showing mature cataracts in both eyes.
CONCLUSION
Cataracts in young patients are always a matter for further evaluation. Hypoparathyroidism should always be considered as one of the causes of bilateral cataracts by clinicians and ophthalmologists. An elaborate medical history and laboratory investigations are important for the diagnosis of such cases. Early diagnosis and prompt treatment of hypocalcaemia, increase the likelihood of visual recovery and can save patients from many complications.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- A study to explore the risk factors for the early onset of Cataract in India. Eye. 2009;24:686-94.
- [CrossRef] [PubMed] [Google Scholar]
- Etiology and pathophysiology of hypoparathyroidism: A narrative review. J Bone Miner Res. 2020;37:2586-601.
- [CrossRef] [PubMed] [Google Scholar]
- Hypoparathyroidism and pseudotumor cerebri: An infrequent clinical association. Can J Neurol Sci. 1987;14:622-5.
- [Google Scholar]
- Hypoparathyroidism and pseudohypoparathyroidism: Etiology, laboratory features and complications. Arch Endocrinol Metab. 2016;60:532-6.
- [CrossRef] [PubMed] [Google Scholar]
- Expression of osteogenic molecules in the caudate nucleus and gray matter and their potential relevance for basal ganglia calcification in hypoparathyroidism. J Clin Endocrinol Metab. 2014;99:1741-8.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral papilledema in hypocalcemia. Delhi J Ophthalmol. 2012;23:127-30.
- [CrossRef] [Google Scholar]
- Cerebrospinal fluid absorption in primary hypoparathyroidism. J Neurol Neurosurg Psychiatry. 1977;40:1015-7.
- [CrossRef] [PubMed] [Google Scholar]
- Papilledema and idiopathic intracranial hypertension. Contin Lifelong Learn Neurol. 2014;20:857-76.
- [CrossRef] [PubMed] [Google Scholar]
- Optic disc involvement in hypocalcaemia with hypoparathyroidism: Papilloedema or optic neuropathy? Neuro Ophthalmol. 1998;20:117-24.
- [CrossRef] [Google Scholar]
- Characteristic cataract associated with idiopathic hypoparathyroidism. J Clin Exp Ophthalmol. 2016;7:4.
- [CrossRef] [Google Scholar]







