Translate this page into:
Safety and efficacy of phacoemulsification and intraocular lens implantation through a small pupil using iris retractors
*Corresponding author: Dr. Anu Kumari, Junior Resident, Department of Ophthalmology, Mahatme Eye Bank and Eye Hospital, Nagpur, Maharashtra, India. anukumari142@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Kumari A, Wairagade NA. Safety and efficacy of phacoemulsification and intraocular lens implantation through a small pupil using iris retractors. Glob J Cataract Surg Res Ophthalmol. 2024;3:58-65. doi: 10.25259/GJCSRO_12_2024
Abstract
Objectives:
The objectives of this study were to study the postoperative (postop) outcome of phacoemulsification using iris retractors in patients with small pupils and compare it with well dilating pupils by comparing the final visual acuity, intra- and post-operative complications, endothelial cell count, and anterior chamber (AC) depth of patients with small pupil with those of well-dilated pupil.
Materials and Methods:
This was a prospective cross-sectional study for December 2020–March 2022 which included 86 eyes of 86 patients. For study purposes eyes were divided into two groups, Group 1 consisted of 43 subjects with post-mydriatic dilatation (≤5 mm), and Group 2 consisted of 43 cases with well-dilated pupils ≥6 mm.
Results:
Group 1 intraoperatively difficulties faced – incomplete rhexis or runoff (41.86%, n = 43), incomplete nucleus chopping (32.55%, n = 43) and retained cortical matter (46.51%, n = 43) noted, managed by applying iris retractors while group 2 faced no difficulties during surgery. In group 1, 33 patients (76.74%) had no complications. Retained cortex was seen in 5 patients (11.62%) and was the most common complication. In group 2, 41 patients (95.34%) had uneventful cataract surgery while 2 patients (4.64%) had minimally retained cortex on post op day 1. Best-corrected visual acuity (BCVA) – 3 months follow-up was good (Snellen-6/6–6/18, logMar 0.00–0.48) in 90.7% in group 1 and 97.7% in group 2. BCVA was borderline (Snellen 6/24–6/60, logMar 0.60–1.00) in 9.30% in group 1 and 2.32% in group 2. Group 1 mean pre-operative endothelial cell density (2528.44 ± 61.26) in group 2 (2457.05 ± 91.17) was significant. On postop day 1 ,1 week and at 3 months endothelial cell density decreased by 4.27%,7.75%,11.92% respectively compared to preoperative values in group 1 while in group 2 it decreased by 2.20%,3.84%,5.40% respectively compared to preoperative values. AC depth was shallower (2.49 ± 0.39) in patients in which complication was noted compared to AC depth (2.72 ± 0.41) in which there was no complication, P value being 0.010 is significant.
Conclusion:
Small pupil poses some difficulty in cataract surgery which can be overcome by timely intervention by expert surgeons and complication rates can be minimised.
Keywords
Cataract
Small pupil
Iris hooks
Phacoemulsification
Lens
INTRODUCTION
Cataract is the most common aetiology of visual impairment in the elderly and represents the reversible cause of preventable blindness worldwide.[1] Clear corneal cataract surgery has now become a common practice since ophthalmologists started using topical anaesthesia, phacoemulsification, and small foldable intraocular lenses (IOLs) during the past two decades.[1,2] Cataract surgery through small corneal incisions (<3.0 mm) requires high technical skills to perform safe and successful cataract surgery without increasing any risk of corneal, iris, or capsular damage. Some patients who require cataract surgery have eyes with non-dilating pupils, which can be attributed to aging, diabetes, pseudoexfoliation (PEX), uveitis, use of miotic agents, glaucoma, trauma, or any previous intraocular surgical surgeries. Studies have estimated that small pupil cataracts account for approximately 11% of all cataract surgeries. Small pupils can hamper visualisation and can bring about notable difficulties in handling intraocular instruments, leading to inadequate or incomplete capsulorhexis. There is a high risk of other complications while doing phacoemulsification through a small pupil, such as iris sphincter tear, intraocular bleeding, rupture of the posterior capsule, vitreous loss[1,3], and loss of endothelial cells.[4] The above-mentioned possible intraoperative difficulties and complications can result in complaints of photophobia, permanent ocular aches, and pupillary irregularities. A pre-operative small pupil that does not dilate with mydriatics should be differentiated from intraoperative constriction of the pupil which can occur due to iris tissue manipulation. The use of non-steroidal anti-inflammatory drugs (NSAIDs) preoperatively has also been shown to support mydriasis and/or prevent miosis.[5-7] Even so, the problem of miosis during cataract surgery remains a relatively common occurrence. The pupil may fail to dilate in conditions such as PEX, after long-term miotic treatment for glaucoma, after trauma or surgery.[8] All these eyes are more prone to increased permeability of blood-aqueous barrier which can lead to postoperative (postop) inflammation.[9] Cataract surgery in eyes with small anterior segments poses a significant challenge to the finest surgeons. Furthermore, the size of the pupil, the age of the patient, the nuclear hardness, the type of cataract, other associated ocular pathologies, the refractive status, and the anterior chamber (AC) depth all collectively add to the possibility of complications. There is no consensus in the current literature on what size of the pupil is insufficient to proceed with cataract surgery. In some studies, the diameter of the pupil to be considered small may start from 6.0 mm.[10] Due to poorer pupil dilation and increased zonular instability, cataract surgery with PEX is associated with a 5-–10-fold increase in surgical complications compared to cataract surgery without PEX.[11] Multiple methods that stretch small pupils mechanically have also been discovered. These comprise the use of a blade, needle and scissors to create several iris sphincter tears.[12] Alternatively, iris retractors and rings can also be used to retract the iris through corneal stab incisions[13] or mechanical stretching devices can be inserted to pull the iris sphincter.[2,13,14] All these methods necessitate sophisticated instruments and demand difficult intraocular manoeuvres, which can incur postop bleeding, and an abnormal pupil shape and can also damage functions of the iris sphincter.[1] Correct use of these rings and retractors can help us by providing a proper field of view during surgery and also help us avoid unwanted complications. To avoid all the above-mentioned undesirable effects in patients having small pupils, and also to study their safety and efficacy, we compared and studied the outcomes of phacoemulsification through a small pupil using minimum iris manipulation and through a normal pupil performed by experienced surgeons.
MATERIALS AND METHODS
It was a prospective cross-sectional study done between December 2020 and March 2022 at a tertiary centre in Central India which included 86 eyes that underwent phacoemulsification for treatment of cataract. Iris retractors were used in patients having small pupils. For study purposes eyes were divided into two groups, Group 1 consisted of 43 subjects with post-mydriatic dilatation (≤5 mm), and Group 2 consisted of 43 cases with well dilated pupils ≥6 mm. After obtaining the informed consent, demographic data of patients were collected including name, age, sex, occupation, and personal details. The ophthalmologic examination included best-corrected visual acuity (BCVA) (using Snellen’s chart and logarithm of the minimal angle of resolution (Log MAR) charts), slit-lamp biomicroscopy, and assessment of the retina by indirect ophthalmoscopy. Log MAR charts were used in this study for recording visual acuity as these charts have become the gold standard method for recording visual acuity in clinical studies. Visual acuity with Snellen chart at 6 m (6/6), at 20 feet (20/20), 1.0 vision in decimal charts, and 0.0 log MAR are considered equivalent. Pupil diameter was measured using a slit-lamp, and an average of vertical and horizontal diameter was taken. Patients with pupil diameter ≤5 mm were placed in group 1, another group 2 consisted of patients with pupil diameter ≥6 mm to compare the results of the phacoemulsification procedure in the two groups. Pupillary reaction to the light stimulus was noted by looking at the minimum pupillary area before and after the light stimulus. The contraction rate of the pupil in response to the light stimulus was noted in both groups. Routine tests complete blood count, electrocardiogram, random blood sugar, blood pressure, and pre-anaesthetic check-up done in all cases. If any comorbid conditions were found, they were managed before surgery after consultation from the concerned specialist, and proper precautions were taken before, during, and after surgery. Anticoagulants if any were stopped 5 days before surgery. Patients underwent phacoemulsification surgery after biometry. Only one eye of each patient was scheduled for cataract surgery. One experienced surgeon performed all procedures according to a standardised protocol. It was done under peribulbar anaesthesia, 5 mL of 2% lignocaine with hyaluronidase was used. Small pupils were managed by iris hooks by pushing and pulling the iris stretching first horizontally then vertically. The iris hooks were applied before the start of capsulorhexis until the IOL was implanted and subsequently removed. Pupil size was measured horizontally preoperatively, and also, after the patient was taken inside the operation theatre and decision to use the iris hooks was made. Intraoperative difficulties and complications were noted. Patients received standard postoperative care. Patient follow-up was done on postop day 1, 1st week, and 3 months of post-operation. During follow-up, patients were subjected to visual acuity testing, anterior segment examination under slit-lamp, and posterior segment examination under indirect ophthalmoscope. The final status of the eye including uncorrected and best-corrected visual acuity was noted at the end of 3 months following surgery.
The formula for determining sample size in this case is given below:
Comparison of proportions (Chi-square test)
Where
P1 = Anticipated proportion in group 1
P2 = Anticipated proportion in group 2 (control)
Z(1-α/2) = 1.96
Z(1-β/2) = 0.84 for 80% power
Thus sample size is 74 cases, which was rounded off as 75 cases. Considering total loss to follow-up as 15% sample size of the study is taken as 86.
RESULTS
Source of data-The study was done in eyes that underwent phacoemulsification for treatment of cataract.Iris retractors were used in patients having semi dilated pupils.
Table 1 shows the difficulty encountered intraoperatively in both significant groups. The above difficulties were overcome after applying iris retractors which led to proper visualisation of the structures.
| Systemic history | Group 1 (43) | Group 2 (43) | P-value | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Poor visualisation of structures behind iris plane | |||||
| Yes | 43 | 100% | 00 | 00 | <0.001 |
| No | 00 | 00% | 43 | 100% | |
| Incomplete rhexis | |||||
| Yes | 18 | 41.86% | 00 | 00 | <0.001 |
| No | 25 | 58.13% | 43 | 100% | |
| Incomplete nucleus chopping | |||||
| Yes | 14 | 32.55% | 00 | 00 | <0.002 |
| No | 29 | 67.44% | 43 | 100% | |
| Incomplete cortex wash | |||||
| Yes | 20 | 46.51% | 00 | 00 | <0.001 |
| No | 23 | 53.48% | 43 | 100% | |
Table 2 shows the intraoperative complications observed in both groups which were not significant.
| Type of complication noted | Group 1 (43) | Group 2 (43) | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Nil | 33 | 76.74% | 41 | 95.34% |
| Posterior capsular rent only | 03 | 6.97% | 00 | 00 |
| Posterior capsular rent with vitreous loss | 01 | 2.32% | 00 | 00 |
| Iris prolapse | 01 | 2.32% | 00 | 00 |
| Retained cortex | 05 | 11.62% | 02 | 4.65% |
| Iridodialysis | 00 | 00 | 00 | 00 |
| Iridodialysis with hyphema | 00 | 00 | 00 | 00 |
Table 3 shows the anterior segment findings on postop day 1 in both groups which are not significant. The most common finding in group 1 was grade 1 iritis (62.79%) followed by grade 1 corneal oedema (53.48%). In group 2, the most common finding on day 1 was found to be grade 1 corneal oedema (62.79%) while grade 1 iritis was found in 55.81% of cases.
| Anterior segment findings | Group 1 (43) | Group 2 (43) | P-Value | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Corneal edema | |||||
| Grade 0 | 05 | 11.62% | 10 | 23.25% | 0.118 |
| Grade 1 | 23 | 53.48% | 27 | 62.79% | |
| Grade 2 | 12 | 27.90% | 06 | 13.95% | |
| Grade 3 | 03 | 6.97% | 00 | 00 | |
| Iritis | |||||
| Grade 0 | 12 | 27.90% | 18 | 41.86% | 0.204 |
| Grade 1 | 27 | 62.79% | 24 | 55.81% | |
| Grade 2 | 04 | 9.30% | 01 | 2.32% | |
| Grade 3 | 00 | 00 | 00 | 2.32% | |
| Streak hyphema | |||||
| Yes | 05 | 11.62% | 01 | 00 | 0.090 |
| No | 38 | 88.37% | 42 | 97.67% | |
| Iris sphincter tear | |||||
| Yes | 06 | 13.95% | 02 | 4.65% | 0.137 |
| No | 37 | 86.04% | 41 | 95.34% | |
| Retained cortex | |||||
| Yes | 05 | 11.62% | 02 | 4.65% | 0.236 |
| No | 38 | 88.37% | 41 | 95.34% | |
Table 4 compares 3 months of anterior segment findings in both the groups. About 76.74% of cases in group 1 and 90.69% of cases in group 2 were found to have normal anterior segment findings.
| 3 Months anterior segment findings | Group 1 (43) | Group 2 (43) | ||
|---|---|---|---|---|
| Number | % | Number | % | |
| Normal | 33 | 76.74% | 39 | 90.69% |
| Iris pigments on endothelium | 02 | 4.65% | 01 | 2.32% |
| Optic capture | 00 | 00 | 00 | 00 |
| Retained cortex behind the lens | 00 | 00 | 00 | 00 |
| Pigments on lens | 02 | 4.65% | 01 | 2.32% |
| Sphincter tear | 06 | 13.95% | 02 | 4.65% |
Table 5 shows the best-corrected visual acuity of both the groups on postop day 1, 1 week, and 3 months which are not significant. Good vision was reported in 30.23% of cases of group 1 on postop day 1 which increased to 90.7 at the end of 3 months while, in group 2, 46.51% cases reported good vision on day 1 which increased to 97.7% at the end of 3 months.
| Bcva | Post-operative day 1 | Post-operative 1 week | Post-operative 3 months | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group 1 | (43) | Group 2 | (43) | Group 1 | (43) | Group 2 | (43) | Group 1 | (43) | Group 2 | (43) | |
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| 1.Good Snellen (6/6-6/18) | 13 | 30.23% | 20 | 46.51% | 29 | 67.44% 35 | 81.39% | 39 | 90.7% | 42 | 97.7% | |
| Logmar (0.00-0.48) | ||||||||||||
| 2.Borderline (6/24-6/60) | 27 | 62.79% | 23 | 53.48% | 14 | 32.55% | 08 | 18.6% | 04 | 9.30% | 01 | 2.32% |
| Logmar (0.60-1.00) | ||||||||||||
| 3.Poor (<6/60) Logmar (>1) | 03 | 6.97% | 00 | 00 | 00 | 00 | 00 | 00 | 00 | 00 | 00 | 00 |
| P-Value | 0.223 | 0.138 | 0.166 | |||||||||
BCVA: Best-corrected visual acuity
Table 6 shows the Endothelial cell density (ECD) values in cells/mm2. There was a significant difference observed in pre-operative values in both groups. Furthermore, there was a decrease in cell count observed in both groups postoperatively which was significant.
| Endothelial cell density (ECD) values | Group 1 | Group 2 | P-Value | ||
|---|---|---|---|---|---|
| Mean | Standard deviation (SD) | Mean | Standard deviation (SD) | ||
| Preoperative | 2528.44 | 61.26 | 2457.05 | 91.17 | 0.001 |
| Postoperative (At 1 Day) | 2420.30 | 49.67 | 2402.79 | 83.27 | <0.001 |
| Postoperative (At 1 Week) | 2332.30 | 44.93 | 2362.53 | 75.35 | <0.001 |
| Postoperative (At 3 Months) | 2226.95 | 55.24 | 2324.30 | 74.99 | <0.001 |
ECD: Endothelial cell density, SD: Standard deviation
Table 7 shows a percentage change in endothelial cell density postoperatively in both groups compared to pre-operative values. The mean AC depth in patients in which complication was noted was 2.49 ± 0.39. The mean AC depth in patients in which there was no complication was 2.72 ± 0.41 P = 0.010 which is significant.
| Group 1 | Group 2 | |
|---|---|---|
| Postoperative Day 1 | 4.27% | 2.20% |
| Postoperative 1St Week | 7.75% | 3.84% |
| Postoperative 3 Months | 11.92% | 5.40% |
DISCUSSION
The present study was conducted to evaluate the safety and efficacy of phacoemulsification and IOL implantation through a small pupil using iris retractors. The study was conducted in a teaching institute on patients with senile cataracts during the study period of December 2020–March 2022. A sample size of 86 eyes was enrolled for the study. A detailed examination of the patient was done. After a detailed ocular examination of patients, inclusion and exclusion criteria were applied and patients were selected and grouped according to their pupil size.
Intraoperative difficulties
In all 43 cases in group 1, the visualisation of structures behind the plane of the iris was compromised and led to difficulties in further steps. Performing capsulorhexis was difficult in 41.86% of the cases, problems which were encountered were – capsular splitting phenomenon, peripheral run, and incomplete capsulorhexis which were quite difficult to identify due to poor visualisation and small rhexis which required relaxing cuts. Incomplete nucleus chopping was seen in 32.55%, complications such as peripheral extension of the relaxing cuts of rhexis and posterior capsular (PC) rent were encountered during this step. Cortical wash was incomplete, and hence, the retained cortex was seen in 46.51% of the cases. Visualising rhexis margin was difficult due to a small pupil with a disturbed cortex that led to PC rent and iris trauma. To minimize further complications, iris retractors were used in all 43 cases. In group 2, however, no such intraoperative difficulties were encountered in any of the 43 cases.
Intraoperative complications in group 1 surgery were uneventful in the majority of the patients (76.74%). PC rent was seen at 6.97%. One patient (2.32%) had PC rent with vitreous loss. The majority of the complications (11.62%) included a minimal amount of retained cortex, without aspiration with suspicion of zonular dehiscence in that position. PC rent was noted during cortical wash as visibility was hampered with disturbed dense cortical matter. Complication was identified at its initial stage and vitreous loss was prevented in these cases except in one case where mild vitreous loss was noted. The vitreous loss was managed with anterior vitrectomy. In all two of four cases with stable capsular bags, IOL was placed in the sulcus. In two cases of central small rent, IOL was placed in the bag.
In group 2, no PC rent was noted as the visualisation of structures behind the iris plane was not hampered. Figure 1 compares intraoperative complications in a similar study. Pranathi et al.[15] included only PEX cases whereas in this study, all cases with small pupils fulfilling inclusion criteria were included in the study.
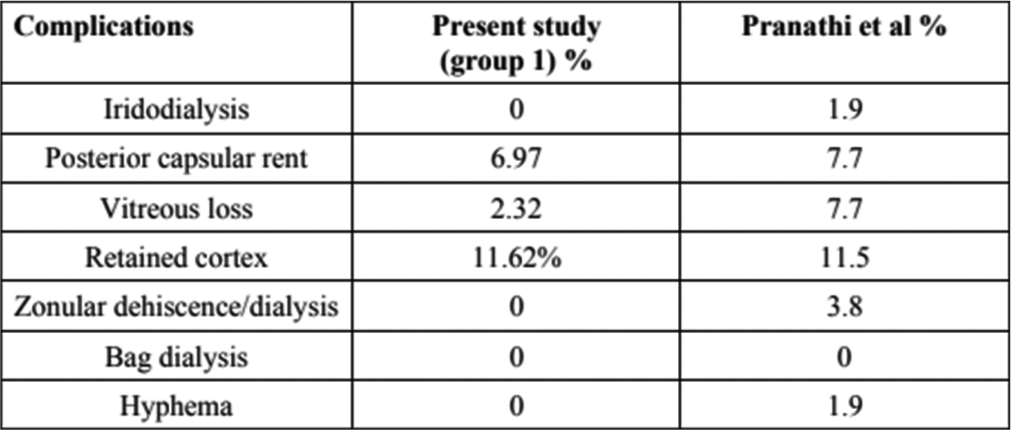
- Intraoperative complications in a similar study.
Anterior segment findings on post-operative day 1. In group 1, 11.62% had clear cornea on post-operative day 1. The rest of the patients had varying grades of corneal oedema. Figure 2 shows a comparison of post-operative day 1 corneal oedema between the present study and Papaconstantinou et al.[1]
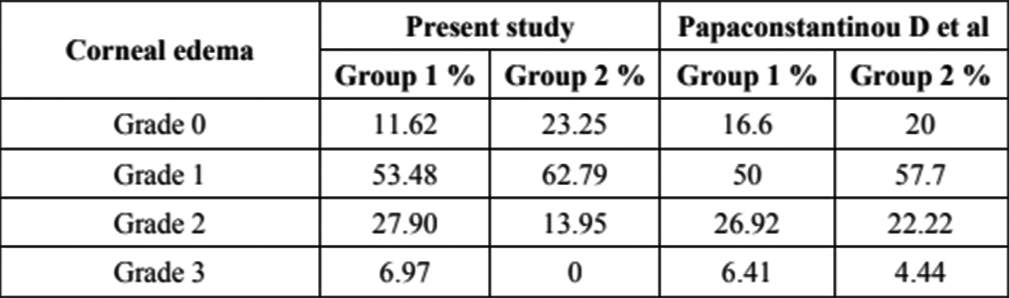
- Comparison of post-operative day 1 corneal oedema between the present study and Papaconstantinou et al.
The results obtained in the present study and in the study done by Papaconstantinou D et al were almost similar.[1] The most common AC finding in group 1 cases was postoperative iritis grade 1 (62.79%). In a study, it was found that post-operative uveitis was more common among cases with intraoperative iris manipulation.[16] About 11.62% of cases had iris sphincter tear and iris stromal distortion. Five patients had retained cortex which was evident on post-operative day 1. Among these five cases, none of them required cortical wash on the first post-op day 1 as it was minimal and there was spontaneous resolution in later follow-ups. In the study done by Papaconstantinou et al., significant corneal oedema and iritis (grades 2–3) were observed more frequently in group I eyes rather than in group II.[1] In group 2, however, 55.81% had mild iritis postoperatively, sphincter tear was seen in 2 (4.65%) cases, while 2 (4.65%) had minimally retained cortex behind the lens on post-op day 1 3 months of follow-up.[1] At the end of 3 months of follow-up in group 1, 76.74% had a normal anterior segment with a resolution of corneal oedema and post-operative iritis. About 4.65% had iris pigments on the corneal endothelium. The incidence of clinically significant pseudophakic cystoid macular oedema (PCME) in this study is 2 (4.65%) which falls in the range (0.8–20%) as described by Grzybowski et al.,[17] both the cases were treated with topical NSAIDs and topical corticosteroids. No official US Food and Drug Administration-approved strategy for PCME prevention after cataract surgery is available, but an extensive meta-analysis of the literature in 1998 concluded that treatment with NSAIDs is beneficial.[18]
In group 2 at the end of 3 months follow-up, 93% had normal anterior segment findings, 2.32% had iris pigments on endothelium and another 2.32% had iris pigments on the lens, while there was 1 (2.32%) case of sphincter tear. There was a 2.32% incidence of significant macular oedema in group 2, which was relieved by topical drugs.
Visual outcome
In this study in group 1, 30.23% had good vision at postoperative day 1 compared to 46.51% in group 2. About 62.79% in Group 1 had borderline vision on post-operative day 1 while 53.48% in Group 2 had a borderline vision. About 6.97% in group 1 had poor vision while no patient in group 2 had poor vision. There was improvement in vision in group 1 from 30.23% having good vision on post-op day 1–90.7% having good vision at the end of 3 months, while, in group 2, 46.51% had good vision on day 1 post-op which improved to 97.7% at the end of 3 months.
By the end of 3 months, following surgery visual acuity was significantly better. Post-operative best-corrected visual acuity followed the World Health Organization (WHO) target guideline. Figure 3 shows a comparison of BCVA obtained in different studies with the WHO guideline. The final BCVA obtained in this study is less than that seen in the study done by Venkatesh et al.[19] but better than BCVA reported by Pranathi et al.[15] and Olawoye et al.[20] Endothelial cell density - Mean preoperative endothelial cell density in group 1 was 2528.44 ± 61.26 while in group 2 was 2457.05 ± 91.17. On postop day 1, the mean endothelial cell density in group 1 was 2420.30 ± 49.67 while in group 2 was 2402.79 ± 83.27 which had reduced by 4.27% and 2.20%, respectively, compared to the preoperative values, P< 0.001 which is significant. On postop, 1 week, mean endothelial cell density in group 1 was 2332.30 ± 44.93 while, in group 2, it was 2362.53 ± 75.35 which had reduced by 7.75% and 3.84%, respectively, compared to pre-operative values, again P- < 0.001 which is significant. Three months post-op, the mean endothelial cell density in group 1 was 2226.95 ± 55.24 while, in group 2, it was 2324.30 ± 74.99 which had reduced by 11.92% and 5.40%, respectively. A study was done by Beato et al.[21] to compare the corneal structure and endothelial morphological features between patients with type 2 diabetes mellitus (DM) and non-diabetic patients; 60 diabetic patients and 47 age- and sex-matched controls were enrolled in this cross-sectional study. There were no statistically significant differences in the endothelium cell density or morphology between DM and non-DM groups (P > 0.05).
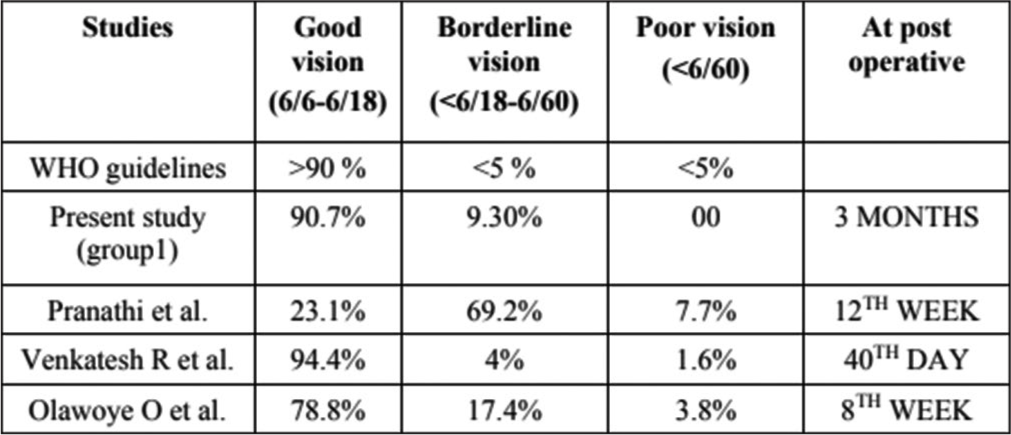
- Comparison of best-corrected visual acuity (BCVA) different studies with World Health Organization (WHO) guidelines.
AC depth in group 1 mean AC depth was 2.64 ± 0.40, while, in group 2, it was 2.74 ± 0.42, P-= 0.286 which is not significant. However, cases in which complications were noted had shallower AC depth of 2.49 ± 0.39 compared to 2.72 ± 0.41 in which no complications were noted, P-= 0.010 which is significant. In a study to look for associations of preoperative A-scan ultrasound ocular dimensions with complications during phacoemulsification in eyes with PEX done by Küchle et al., it was found that the AC depth was shallower in eyes with complications than in eyes without complications (mean, 2.36 ± 0.44 mm vs. 2.74 ± 0.52 mm; P = 0.013).[22]
Strengths and limitations of the study
The strength of our study is that it is a prospective study with different kinds of cases including ocular comorbidities. Furthermore, ours is a teaching training institute where the volume of surgeries done every day is high with limited resources. The results obtained are at par with the published literature. The study has several limitations too. We could not grade the severity of underlying eye diseases. Furthermore, we did not collect data regarding patient-reported outcomes so patient satisfaction is not taken into account in this study.
CONCLUSION
Small pupil poses some difficulty in most of the steps of cataract surgery which can be overcome by timely intervention by expert surgeons and thus the complication rates were minimised. Visco-mydriasis was attempted in all cases and iris hooks were used. Most common intra-operative complications in this study were retained cortex due to poor visualisation which can be minimised by using iris retractors. Intra-operative miosis adds on to the difficulty posed by small pupils. Visual impairment on immediate post-operative day 1 is mainly due to corneal edema and iritis. Proper and careful preoperative evaluation, foreseeing difficulties and being prepared for it and with timely intervention good results can be achieved. Also stratifying the cases on the basis of risk factors associated helps in better preparedness while doing surgery also in proper counselling of the patients pre-operatively.
Ethical approval
The research/study was approved by the Institutional Ethics Committee at Mahatme Eye Bank and Eye Hospital, number 2066144068, dated 8/12/2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Safety and efficacy of phacoemulsification and intraocular lens implantation through a small pupil using minimal iris manipulation. Clin Interv Aging. 2016;11:651-7.
- [CrossRef] [PubMed] [Google Scholar]
- Management of the small pupil for clear corneal cataract surgery. J Cataract Refract Surg. 2002;28:1826-31.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for intraoperative complications in 1000 extracapsular cataract cases. Ophthalmology. 1987;94:461-6.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for corneal endothelial injury during phacoemulsification. J Cataract Refract Surg. 1996;22:1079-84.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety profile of ketorolac 0.5% ophthalmic solution in the prevention of surgically induced miosis during cataract surgery. Clin Ther. 1999;21:723-32.
- [CrossRef] [PubMed] [Google Scholar]
- Inhibition of surgically induced miosis and prevention of postoperative macular edema with nepafenac. Clin Ophthalmol Auckl NZ. 2009;3:219-26.
- [CrossRef] [PubMed] [Google Scholar]
- Management of mydriasis and pain in cataract and intraocular lens surgery: Review of current medications and future directions. Clin Ophthalmol Auckl NZ. 2014;8:1281-9.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence and predictors of ocular complications associated with cataract surgery in United States veterans. Ophthalmology. 2011;118:507-14.
- [CrossRef] [PubMed] [Google Scholar]
- Surgically induced miosis during phacoemulsification in patients with diabetes mellitus. Eye Lond Engl. 2003;17:194-9.
- [CrossRef] [PubMed] [Google Scholar]
- Intracameral ketorolac and phenylephrine effect on intraoperative pupil diameter and postoperative pain in cataract surgery. J Cataract Refract Surg. 2017;43:597-605.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudoexfoliation syndrome and pseudoexfoliation glaucoma. J Fr Ophtalmol. 2018;41:78-90.
- [CrossRef] [PubMed] [Google Scholar]
- Pupilloplasty for small pupil phacoemulsification. J Cataract Refract Surg. 1994;20:192-6.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of various pupil dilatation methods for phacoemulsification in eyes with a small pupil secondary to pseudoexfoliation. Ophthalmology. 2004;111:1693-8.
- [CrossRef] [PubMed] [Google Scholar]
- Small pupil phaco surgery: A new technique. Ann Ophthalmol Skokie Ill. 2007;39:185-93.
- [CrossRef] [PubMed] [Google Scholar]
- A study of complications during cataract surgery in patients with pseudoexfoliation syndrome. J Clin Ophthalmol Res. 2014;2:7-11.
- [CrossRef] [Google Scholar]
- Pupillary autonomic denervation with increasing duration of diabetes mellitus. Br J Ophthalmol. 2001;85:1225-30.
- [CrossRef] [PubMed] [Google Scholar]
- Pseudophakic cystoid macular edema: Update 2016. Clin Interv Aging. 2016;11:1221-9.
- [CrossRef] [PubMed] [Google Scholar]
- Medical prophylaxis and treatment of cystoid macular edema after cataract surgery. The results of a meta-analysis. Ophthalmology. 1998;105:397-405.
- [CrossRef] [PubMed] [Google Scholar]
- Outcomes of high volume cataract surgeries in a developing country. Br J Ophthalmol. 2005;89:1079-83.
- [CrossRef] [PubMed] [Google Scholar]
- Visual outcome after cataract surgery at the university college hospital, Ibadan. Ann Ib Postgrad Med. 2011;9:8-13.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of corneal structure and endothelial morphological characteristics in type 2 diabetic and non-diabetic patients. Clin Ophthalmol Auckl NZ. 2020;14:1993-9.
- [CrossRef] [PubMed] [Google Scholar]
- Anterior chamber depth and complications during cataract surgery in eyes with pseudoexfoliation syndrome. Am J Ophthalmol. 2000;129:281-5.
- [CrossRef] [PubMed] [Google Scholar]






