Translate this page into:
Target emmetropia – Ocular surface stabilisation and achieving refractive success with a new presbyopia-correcting intraocular lens
*Corresponding author: Sony Sinha, Department of Ophthalmology, All India Institute of Medical Sciences, Patna, Bihar, India. nishanteyecare@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sinha S, Nishant P, Kumar R, Rajendra AS. Target emmetropia – Ocular surface stabilisation and achieving refractive success with a new presbyopia-correcting intraocular lens. Glob J Cataract Surg Res Ophthalmol. 2025;4:35-9. doi: 10.25259/GJCSRO_30_2024
Abstract
Recent advancements in intraocular lens (IOL) technology enable us to cater to the visual needs of demanding patients. A 53-year-old woman presented with a history of using heavy eye makeup and bilateral Nuclear Sclerosis Grade II (NS-II) cataracts. On examination, corrected distance visual acuity in both eyes was 6/6 and near visual acuity was N6. Both eyes had grade II meibomitis and dry eye. Being hypermetropic, she wanted complete spectacle-independence. As a boutique owner, her visual demands included fine tailoring work. The decision to use a presbyopia-correcting IOL was deferred due to a diseased ocular surface. Spectacles were prescribed and meibomitis and dry eye were treated. Pentacam values and IOL master calculations changed during her treatment over 6 months. Finally, with a stable ocular surface, both eyes underwent surgery with Adtec Xtnd IOL and achieved uncorrected visual acuity of 6/6 N6. Refractive success can be achieved with modern presbyopia-correcting IOLs in demanding patients with ocular surface disease.
Keywords
Cataract
Dry eye syndrome
Intraocular lens
Meibomian gland disease
Visual acuity
INTRODUCTION
Recent advancements in intraocular lens (IOL) technology enable us to cater to the visual needs of demanding patients. Requests for refractive correction of presbyopia along with cataract surgery can be attributed to the increase of younger patients who demand a solution for their presbyopia and look for spectacle-independence.[1]
It has been found in previous studies that appropriately selected patients can achieve spectacle-independence and good visual satisfaction with presbyopia-correcting IOLs. The process includes proper patient education, a comprehensive evaluation of patients’ lifestyle and personality dynamics and an individualised weighing of benefits and side effects of such IOLs.[2]
However, the refractive success of presbyopia-correcting IOLs is limited by factors that limit accurate IOL power calculation, as well as the tendency of these IOLs to cause photic symptoms and sometimes the cost. These factors are summarised into a list of red-flag attributes, in which these IOLs are traditionally avoided.[3,4]
We, hereby, present the case of a patient who, despite several red-flag attributes, received a modern hybrid (extended depth of focus [EDOF] + trifocal) IOL and achieved refractive success due to meticulous pre-operative planning and prior management of comorbidities related to the ocular surface.
CASE REPORT
A 53-year-old female presented with complaints of frequent change of glasses and painless progressive diminution of vision in both eyes. She had been wearing thick plus-powered spectacles all her life and had been using bifocal glasses for presbyopia for the past decade. She had no chronic systemic illnesses but a history of using heavy eye makeup since her teenage, along with the occasional use of contact lenses.
On examination, unaided visual acuity was 6/60 in the right eye (RE) and 6/36 in the left eye (LE), while corrected distance visual acuity in both eyes was 6/6 and corrected near visual acuity was N6. Adnexae had heavy deposits of kohl and glitter. Both eyes had grade II meibomian gland disease (MGD) and moderate dry eye. Pupils were round, regular and symmetrically reactive to light. Both eyes had Nuclear Sclerosis Grade II (NS-II) cataracts. Fundi were unremarkable. Intraocular pressures, ocular motility and stereoacuity, were within normal limits. The rest of the parameters are listed in Table 1. Staining of the ocular surface showed decreased tear-film breakup time (TBUT). Ocular biometry was performed using IOL Master 700 (Carl Zeiss Meditec, Jena, Germany), which showed similar biometric parameters for both eyes. However, Scheimpflug imaging using Pentacam AXL (Oculus Optikgeräte GmbH, Wetzlar, Germany) showed an irregular anterior corneal surface and an unfavourable estimated corneal aberration profile.
| Parameter at presentation | Right eye | Left eye |
|---|---|---|
| Old spectacles | +4.50 DS | +4.50 DS |
| Near add | +1.00 DS | +1.00 DS |
| Acceptance for distance | +2.25 DS 6/6 | +2.25 DS 6/6 |
| Near add acceptance (33 cm) | +2.00 DS N6 | +2.00DS N6 |
| Specular cell density (/mm2) | 2986 | 2885 |
| Pupil diameter | 4.75 mm | 5 mm |
| Pentacam chord µ | 0.6 | 0.4 |
| Chang-Waring chord | 0.4 | 0.4 |
| OCT macula | Within normal limits | Within normal limits |
OCT: Optical coherence tomography, DS: Diopter sphere
The patient was advised sequential cataract surgery in both eyes, with 2.2 mm phacoemulsification and monofocal IOL implantation as the recommended choice of procedure. However, being hypermetropic, she wanted complete spectacle-independence. As a boutique owner, her visual demands included fine tailoring work. Although a comprehensive personality assessment was not performed, she seemed to have Type-A personality traits. The decision to use a presbyopia-correcting IOL was deferred due to a diseased ocular surface.
Spectacles were prescribed and meibomitis and dry eye were treated. Warm compresses and lid massage twice a day were advised, along with eyelid cleaning with sodium hypochlorite-based cleaning solution twice a day, tablet doxycycline 100 mg twice daily for 4 weeks, preservative-free eyedrops of sodium hyaluronate 0.1% as well as cyclosporine (CsA) 0.05% 3 times in both eyes (BE) and eye ointment azithromycin 1% to be applied at night before sleep in BE. The patient was asked to avoid eye cosmetics for the entire period of her treatment. She was poorly compliant with this advice; hence, the treatment course was prolonged over the next 6 months. Pentacam values and IOLMaster 700 calculations changed during this period; however, the clinical decision to continue treatment was based on the reduction of ocular surface debris, consistency and expressibility of meibum as well as patient-reported compliance to therapy [Supplementary Table 1].
The decision to proceed with a presbyopia-correcting IOL was taken based on the improvement in the regularity of anterior corneal profile on Scheimpflug imaging, as well as symmetrisation and increased repeatability of the IOL power calculation in both eyes [Figure 1]. The choice of the presbyopia-correcting IOL (trifocal/multifocal/EDOF/hybrid) was made based on a comprehensive assessment of visual needs performed using a questionnaire developed by Johnson and Johnson Vision, USA [Figure 2]. Based on a nearly equal proportion of distance, intermediate and near tasks and preference for intermediate and near vision, a hybrid (EDOF + Trifocal) IOL design was chosen as the preferred IOL. Based on the patient’s ability to afford the IOL, the choices were limited to lenses from Indian manufacturing. Using the Barrett Universal II formula, the IOL power chosen was +22.00DS in both eyes.
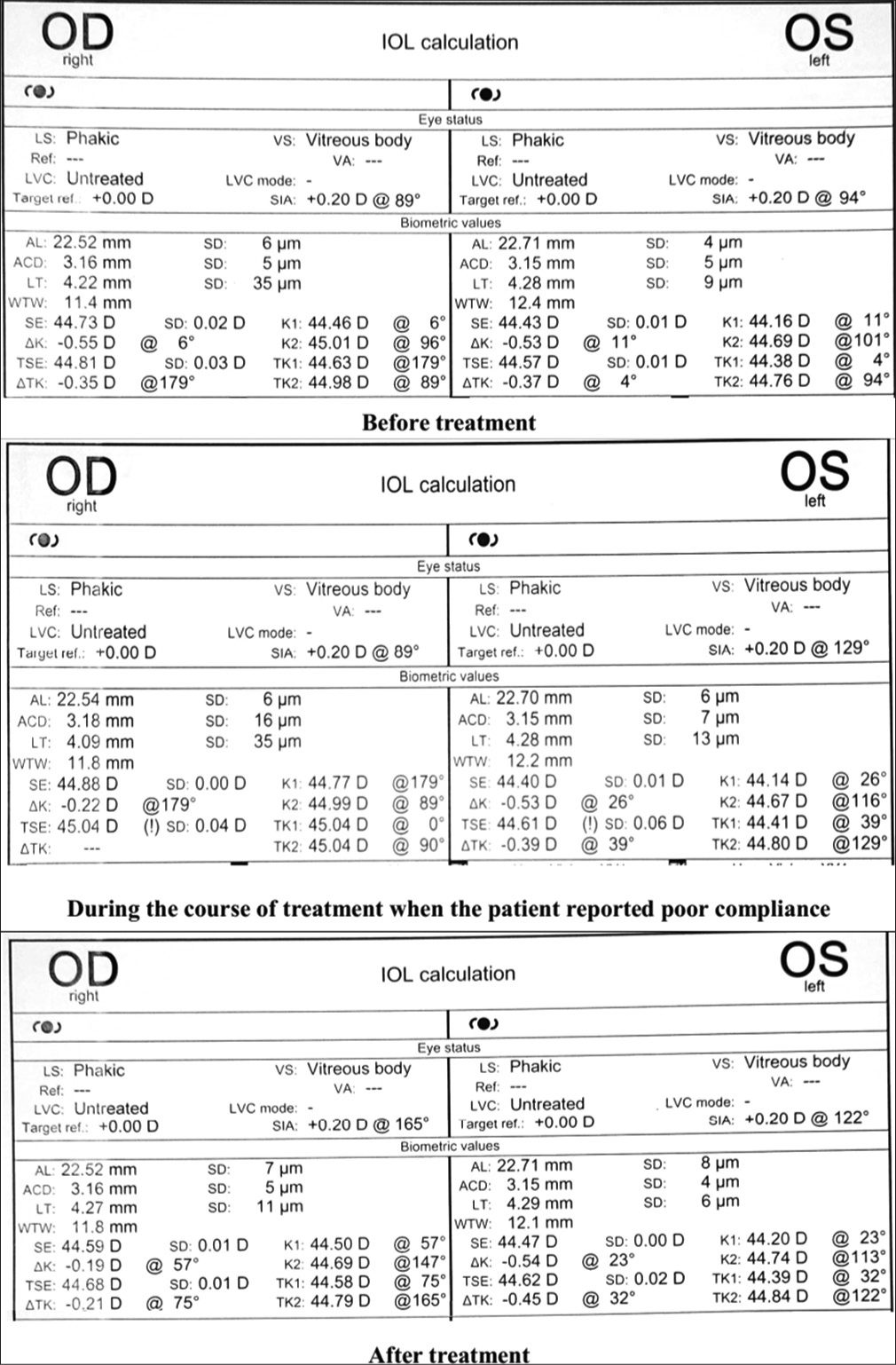
- Intraocular lens master calculations through the course of treatment of the patient. OD: Right eye, OS: Left eye.
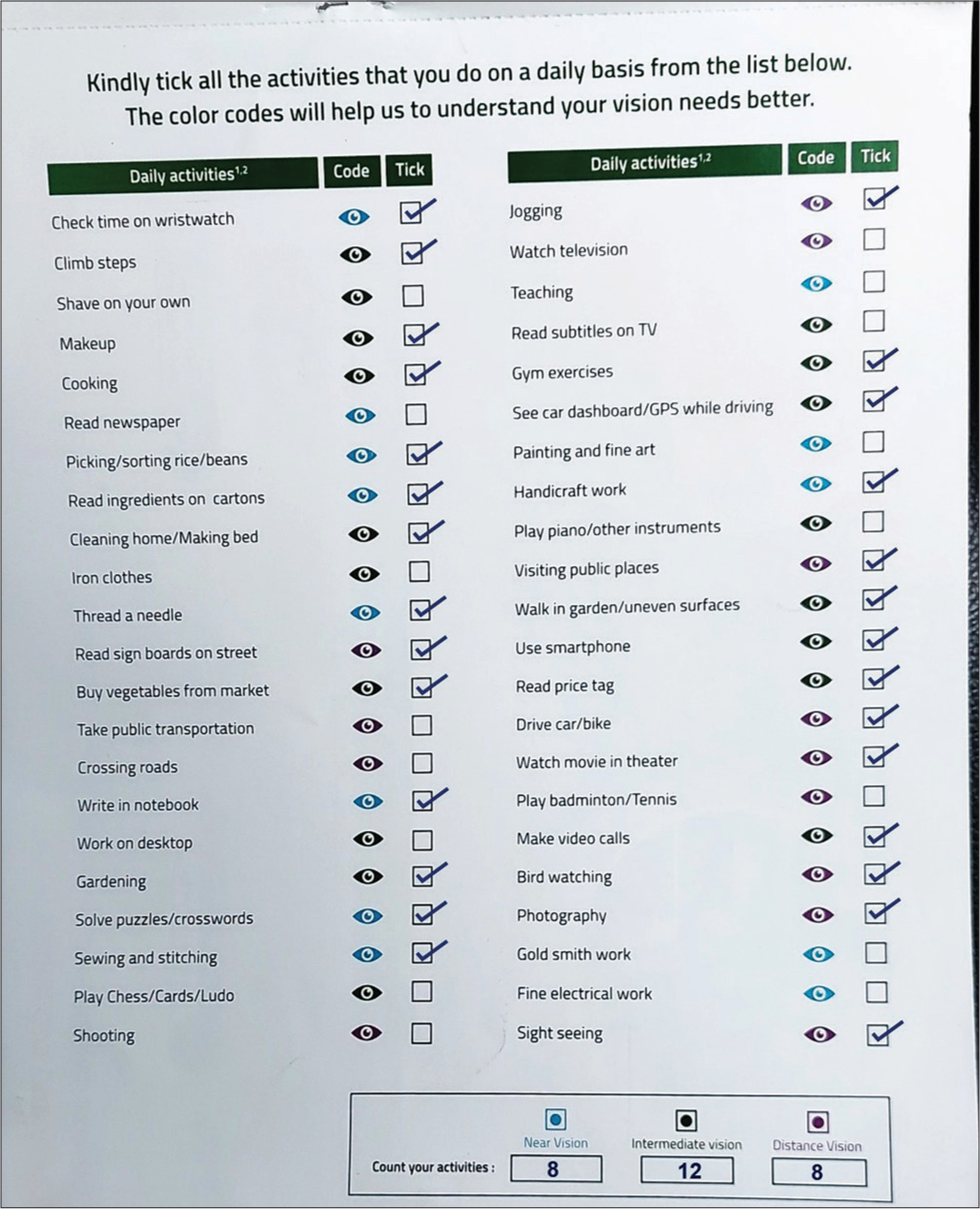
- Johnson and Johnson vision questionnaire for choosing an intraocular lens for the index case. Source: Data on file. JV PP2020CT4270, Johnson and Johnson Vision, USA.
Finally, with stable ocular surface and minimal residual MGD, first, the RE underwent uncomplicated Phacoemulsification surgery with 2.2 mm short post-limbal incision on the (vertical) steep axis, 5.5 mm continuous curvilinear capsulorhexis centred on the visual axis, stop-and-chop nucleofractis, bimanual irrigation and aspiration, along with in-the-bag implantation of the Adtec Xtnd IOL (Adaptive Ocular Technologies, Gujarat, India) under topical anaesthesia (proparacaine eye drops 0.5%). The next day following the surgery, RE had a corrected visual acuity of 6/12 N12 with mild central corneal oedema, and a visual function questionnaire (VFQ)-3oo7 assessment revealed no ocular symptoms.[5]
One week after the surgery, the patient achieved uncorrected visual acuity of 6/6 N6 in RE. Subjective refraction showed no acceptance of spherical or cylindrical power. The same IOL power was implanted in the LE by a similar procedure and achieved 6/6P N6 vision the very next day and 6/6 N6 at a 1-week follow-up. Again, the VFQ-3oo7 assessment revealed no ocular symptoms. There were no complaints regarding disabling reduction of contrast sensitivity as well.
The patient has since completed 12 months of follow-up and has not complained of any dysphotopsia, glare, halos or other visual disturbances and neither of any chronic ocular pain or irritation. Follow-up examinations have shown both IOLs well-centred on the visual axes with no evidence of posterior capsular opacification. The patient has also reduced her tendency to use eye cosmetics indiscriminately and is happy about not having to wear spectacles for any of her daily tasks. She continues to be maintained on sodium hyaluronate 0.1% eye drops 3 times daily in both eyes.
DISCUSSION
As regards the choice of procedure for presbyopia correction in patients with cataracts, it is known that bilateral multifocal IOLs provide better visual results and patient satisfaction postoperatively.[2] Corneal refractive surgical procedures have their concerns and disadvantages and are secondarily performed only in case of failure to obtain the desired refractive outcomes after IOL surgery.[6]
The presbyopia-correcting IOLs include bifocal, trifocal and EDOF IOLs. The EDOF lenses offer better contrast sensitivity and decreased spectacle dependence for distance, intermediate and near vision with lesser visual disturbances compared to bifocal IOLs.[2] The newer category of hybrid IOLs has been recently introduced to provide a continuous range of vision to meet the needs of visually demanding patients.[7,8]
The literature lacks visual outcomes and efficacy studies on the Indian-origin Adtec Xtnd IOL. The recently introduced IOL is a hybrid combining EDOF and trifocal profiles, as well as providing several other benefits. The Adtec IOLs are made from next-generation acrylic material that offers increased tensile strength, enhanced modulus and controlled unfolding due to excellent shape memory. The stiffness of the material allows thinner IOL optics while maintaining compression forces. The material is a copolymer of hydroxyethyl methacrylate and methyl methacrylate and the lens has a modified hydrophobic surface, which, along with the square-edge design, reduces posterior capsular opacification. The material is glistening-free and has high light transmittance, which makes it suitable for use in patients with queer visual demands.[9]
Our case report not only involves the successful implantation of this presbyopia-correcting IOL but also in a patient who could have been deemed otherwise unsuitable for presbyopia-correcting IOLs. The patient was involved in fine near work, showed type-A personality traits, and had a demand for absolute spectacle-independence. She had a poor ocular surface to begin with (grade II MGD as per meiboscore),[10] which may be attributable to chronic ocular surface inflammation resulting from the relentless use of cosmetic products. In addition, her biometry and Scheimpflug data were unreliable at all-time points before ocular surface optimisation, making the choice of type and the power of IOL is difficult. The inclusion of the posterior corneal surface projection of the IOLMaster was critical in determining the IOL power.
It is well known that ocular surface optimisation is essential before cataract surgery, and cataract surgery itself can worsen dry eye.[11,12] The management of MGD is complex. Despite the numerous possible treatment options, it is difficult to obtain complete relief of signs and symptoms. It is known that signs of MGD correlate poorly with symptoms, and the patient was very tolerant of the symptoms, if any, due to her chronic exposure to cosmetics.[13] Thus, no symptoms related to MGD were stated as the presenting complaint; hence, no initial ocular surface disease questionnaire-based evaluation was done.
Two of the important cornerstones in the treatment of MGD in the present case were topical CsA and azithromycin.[14] These adjunctive agents could potentially be the preferred treatment options for MGD arising due to prolonged use of cosmetics; however, this requires further validation. The role of CsA in MGD has been a matter of debate in recent times; very few studies have evaluated real-world evidence regarding the improvement of ocular surface inflammation with CsA.[15] However, the successful treatment of MGD and optimisation of the ocular surface using sodium hyaluronate drops caused enhanced reliability of biometric and Scheimpflug readings, thereby making the patient eligible for presbyopia correction using the IOL. The relatively improved anterior corneal topographic profile of the Scheimpflug image was considered a surrogate marker for the reduction in ocular surface inflammation in the index case.
Finally, this is one of the few case reports utilising the Johnson and Johnson Vision questionnaire for the assessment of the patient’s visual needs, as well as the VFQ-3oo7 questionnaire for patient-reported outcome measures to assess the patient-reported outcomes of IOL surgery. The questionnaire provides a range of tasks that the patients recall as performing during their day, which are then classified as being performed at a distance, intermediate, or near. The questionnaire thus provides an estimate of the proportion of tasks that a patient performs at a given distance, which, thereby, guides IOL choice.[2] The VFQ (three out of seven) is a condensed version of the VFQ-7 questionnaire, which is itself a condensed version of the VFQ-25 questionnaire. With the advantage of simplicity and time efficiency, we believe that both questionnaires are sufficient in cases such as ours.
Limitations of the present case report include the inability to obtain data on wavefront aberrometry, post-operative assessment of photic phenomena in varying light conditions and the role of neuroadaptation in the refractive success as reported. A comprehensive psychiatric assessment was not performed as it was deemed not required. The comprehensive ocular surface profile of inflammatory markers could not be assessed due to the lack of availability and cost of the related investigations. This is the first report on the use of this IOL and suffers from the inherent lack of generalizability – a single case report cannot comment on the performance of an IOL. Further studies are required to comment on the performance of the IOL in different clinical scenarios.
CONCLUSION
Our case report highlights that proper assessment of visual needs, prior stabilisation of the ocular surface, meticulous corneal assessment and IOL power calculation are mandatory to achieve refractive success with newer technology IOLs. If properly performed, the advantage of spectacle-independence can be offered to patients who are otherwise deemed ineligible for presbyopia-correcting IOLs.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Supplementary files are available on:
Financial support and sponsorship: Nil.
References
- Clinical outcomes with a new design in multifocal intraocular lens: A pilot study. Eye Vis (Lond). 2020;7:38.
- [CrossRef] [Google Scholar]
- A clinical study to assess feasibility, acceptance, and outcome of multifocal intraocular lens in patients with bilateral immature cataract at a tertiary eye care institute. Indian J Ophthalmol. 2020;68:2421-6.
- [CrossRef] [Google Scholar]
- Multifocal intraocular lenses: Types, outcomes, complications and how to solve them. Taiwan J Ophthalmol. 2017;7:179-84.
- [CrossRef] [Google Scholar]
- Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35:992-7.
- [CrossRef] [Google Scholar]
- A very short version of the Visual Function Questionnaire (VFQ-3oo7) for use as a routinely applied patient-reported outcome measure. Acta Ophthalmol. 2020;98:618-26.
- [CrossRef] [Google Scholar]
- Photorefractive keratectomy for correcting residual refractive error following cataract surgery with premium intraocular lens implantation. Taiwan J Ophthalmol. 2018;8:149-58.
- [CrossRef] [Google Scholar]
- Comparison of 3-month visual outcomes of a new multifocal intraocular lens vs a trifocal intraocular lens. J Cataract Refract Surg. 2022;48:1270-6.
- [CrossRef] [Google Scholar]
- Comparison of visual results and optical quality of two presbyopia-correcting intraocular lenses: TECNIS symfony versus TECNIS synergy. Eur J Ophthalmol. 2022;32:3461-9.
- [CrossRef] [Google Scholar]
- Advanced ocular lenses for better vision. Adaptive ocular. Available from: http://aospl.in/products.php [Last accessed on 2024 May 11]
- [Google Scholar]
- Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008;115:911-5.
- [CrossRef] [Google Scholar]
- Ocular surface optimization before cataract surgery. Saudi J Ophthalmol. 2022;36:142-8.
- [CrossRef] [Google Scholar]
- Cataract surgery and dry eye disease: A review. Eur J Ophthalmol. 2020;30:840-55.
- [CrossRef] [Google Scholar]
- Correlation of meiboscale symptom score and sign score for primary meibomian gland dysfunction in Indian eyes-A cross-sectional study. Indian J Ophthalmol. 2022;70:1958-62.
- [CrossRef] [Google Scholar]
- Emerging treatment options for meibomian gland dysfunction. Clin Ophthalmol. 2013;7:1797-803.
- [CrossRef] [Google Scholar]
- Evaporative dry eye disease due to meibomian gland dysfunction: Preferred practice pattern guidelines for diagnosis and treatment. Indian J Ophthalmol. 2023;71:1348-56.
- [CrossRef] [Google Scholar]







