Translate this page into:
Visual outcome of cataract surgery from a free outreach camp among rural areas of Southern-Kaduna, Nigeria
*Corresponding author: Stanley Bulus Sano, Department of Ophthalmology, Kaduna State University, Kaduna, Nigeria. stanley.bulus@kasu.edu.ng
-
Received: ,
Accepted: ,
How to cite this article: Bulus SS, Bakut AS, Diyale PS, Mahmoud Z. Visual outcome of cataract surgery from a free outreach camp among rural areas of Southern-Kaduna, Nigeria. Glob J Cataract Surg Res Ophthalmol 2022;1:15-20.
Abstract
Objectives:
The objectives of the study were to assess the visual outcome of those who underwent free cataract surgery in southern senatorial zone of Kaduna State between September and November 2018, and to identify the causes of poor visual outcome (Visual acuity [VA] <6/60 Post op), suggest ways of improving it and comparing findings of this study with other studies.
Materials and Methods:
An observational study of consecutive patients with dense cataracts and VA >6/60 who underwent manual small incision cataract surgery (MSICS) with intraocular lens implant (IOL). All patients had posterior chamber intraocular lens (PCIOL) implant after cataract extraction except 6 who had anterior chamber intraocular lens. A total of 116 eyes of 116 patients who met the inclusion criteria were recruited for the study but only 109 were followed up for 8 weeks postoperatively. Their VA pre-operative was noted. Postoperatively, 1st day, 1,and 8 weeks presenting VA were noted while best corrected VA (BCVA) at 1 week and 8 weeks were also noted. Information collected was analyzed with Statistical Package for the Social Sciences version 19. A 95% significant confidence interval was used, that is, P < 0.05.
Results:
Age range of patients in this study was 40–80 years with a male to female ratio of 1.02:1. All patients presented pre-operatively with poor vision (VA >6/60) but after surgery 27.3%, 42.2%, and 56.6% of patients had good vision (VA 6/6–6/18) on 1st day, 1 week, and 8 weeks post-operatively, respectively, with a BCVA in 75.6% of study population. Complications such as corneal edema, posterior capsule rent, iris tear, cortical remnants, and uncorrected residual refractive errors contributed to poor visual outcome (VA <6/60) 8 weeks after surgery.
Conclusion:
MSICS was effective in restoring visual loss from cataract. Even though the WHO standard was not achieved in this study, provision of required technology for pre-operative preparation and post-operative follow-up along with improvement in surgical techniques will improve visual outcome after cataract surgery.
Keywords
Cataract
Outreach camp
Cataract surgery
Visual outcome
Public-Private Partnership
INTRODUCTION
Cataract is responsible for 43% of blindness in those 40 years and above in Nigeria with more than 85% preventable with appropriate eye care services.[1,2] Unfortunately, many cataract cases and other visually disabling conditions are concentrated in rural areas where public health services are not optimal.[3]
Despite efforts at reducing cataract, it is increasing at 4–6 million new cases per year.[4] Cataract surgical outreach has been found useful in increasing surgical output with the hope that each operated case will restore vision.[5] However, cataract surgery outcome may not be as good as expected, hence the need for adequate attention to it.[4] Studies in Nepal, China, and India revealed 40–75% cataract surgery outcomes were worse than 6/18 in the operated eye with 21–53% having VA of <6/60.[6-8]
In Sub-Sahara Africa, poor outcome with VA less than 6/60 after cataract surgery often comprises 20% or more in published case series.[9]
Outcome of cataract surgery has been categorized by the WHO into three groups as follows: Good (VA 6/6–6/18), borderline (VA<6/18–6/60), and poor (VA<6/60) with a target of uncorrected good VA in 80% surgeries and poor in less than 5% and a target of corrected VA good in 90% surgeries and poor in less than 5% after 2 months of surgery.[9]
Manual small incision cataract surgery (MSICS) is an improvement over extracapsular cataract extraction with intraocular lens (ECCE + PCIOL) and has been found useful in clearing cataract backlog in developing countries. With training more Ophthalmologists in Nigeria have converted from ECCE to MSICS. This study aims to evaluate the visual outcome of all patients with cataract blindness who had MSICS+ intraocular lens implant (IOL) between September and November 2018 in seven Local Government Areas (LGAs) of Kaduna State (Sanga, Jema’a, Zango Kataf, Kaura, Jaba, Kagarko, and Kachia) and identify causes of poor outcome while suggesting ways to improve visual outcome.
MATERIALS AND METHODS
Study design and setting
This was an observational, descriptive, and longitudinal study involving consecutive patients who presented for free cataract surgery at an outreach camp at Sir Ibrahim Patrick Yakowa General Hospital (SIPYGH) Kafanchan between September and November 2018. The outreach program was sponsored by the Federal Government of Nigeria in collaboration with the Ophthalmological Society of Nigeria and the team consisted of two ophthalmologists, five ophthalmic nurses and two medical assistants.
Patients were screened by experienced ophthalmic nurses from the seven LGAs which constitute the Southern Senatorial zone of Kaduna State. Those with dense cataract responsible for VA less than 6/60 and good pupillary reaction were referred to the base hospital for re-screening using pen torch and direct ophthalmoscope. Blood sugar, hemogram, pressure, and retroviral status were also checked.
The SIPYGH Kafanchan is a secondary health-care provider with facilities for cataract surgery and refraction services. It serves as a referral Centre for all the LGAs of Southern senatorial zone of Kaduna State. Screened patients who met the inclusion criteria were included in the study.
Inclusion and exclusion criteria
Patients with operable cataract that were 40 years and above and those with well controlled systemic diseases such as diabetes or hypertension were also included while those with traumatic or complicated cataract, coexisting glaucoma and those who could not complete follow-up for 2 months postoperative were excluded from the study. Consent for surgery and intra-ocular lens implantation was given by all patients and Helsinki Declaration was adhered to while ethical approval was given by the SIPYGH Ethical Committee on Research.
The study was done in three stages. In the first stage, all eligible patients had their data such as name, age, sex, educational level, income, duration of cataract before surgery, reason for delay in surgery, presenting visual acuity (VA), medical, and ocular history were recorded. All patients had MSICS with posterior capsule intraocular lens (PCIOL) except six patients who had anterior chamber (AC) intraocular lens (ACIOL) as a result of posterior capsule rent with vitreous loss. All surgeries were performed under peribulbar local anesthesia (xylocaine 2% + adrenaline 1:100,000 + hyaluronidase). Intraocular lens was chosen based on subjective assessment of the eyes in which large eyes had lower intraocular lens power while smaller eyes had higher intraocular lens powers implanted since biometry was unavailable. Intraocular lens power used ranged from 19.00 to 21.00DS for PCIOL while 17.50 to 18.00DS were used for ACIOL. Those with bilateral cataract had only one eye operated. One hundred and sixteen patients met the inclusion criteria and were included from the study.
In second stage, 1st day post-operative VA was recorded. Pinhole VA was not recorded because of lack of consistency in the result with pin hole.
In the third stage, 1 week and 2 months presenting VA (PVA) and best corrected VA (BCVA) after surgery were assessed and recorded.
Operational definitions
Cataract: Opacity of the lens responsible for VA less than 6/60
Operable cataract: Cataract in which surgery can restore good vision
Blindness: PVA of less than 3/60 in the better eye
BCVA: VA with corrective lenses
PVA: VA without corrective lenses
Complicated cataract: Cataract coexisting with other ocular condition that affect outcome of cataract surgery
Cataract blindness: Cataract causing VA <6/60
Posterior Capsule rent: Tear of the posterior capsule of the lens with or without vitreous loss
Corneal edema: Swelling of the corneal from excessive fluid which makes it to be hazy with decrease vision
Hyphaema: Blood in the AC which may be from ruptured iris vessels or from conjunctiva vessels
Cortical remnants: Particles of residual lens matter in the AC not removed during cataract surgery
Uveitis: Inflammation of eyes following intraocular manipulations. It can affect either the iris, ciliary body of choroid
Endophthalmitis: Inflammation of the aqueous or vitreous due mostly to infection but may also occur from non-infectious causes, for example, lens matter or toxic agents.
RESULTS
A total of 116 eyes of 116 patients were enrolled into the study. Only 109 eyes of 109 patients were followed up for 2 months postoperatively giving an attrition rate of 6.0%. Seven people were lost to follow-up despite counseling them on the need to come for follow-up.
Age and sex distribution
The age range of patients was 40–80 years with mean age 66.4 ± 7.4 years. There were 55 males and 54 females with a male to female ratio of 1.02:1 [Table 1].
| Age group (years) | Male (%) | Female (%) | Total (%) |
|---|---|---|---|
| 40–50 | 0 (0) | 2 (4) | 2 (2) |
| 51–60 | 5 (9) | 3 (6) | 8 (7) |
| 61–70 | 18 (33) | 18 (33) | 36 (33) |
| >70 | 32 (58) | 31 (57) | 63 (58) |
| Total | 55 (100) | 54 (100) | 109 (100) |
Original
More cataract surgeries were done at 70 years and above with 32 males (58%) and 31 females (57%) operated. At between 40 and 50 years, the only 2 (1.8%) people operated were females while at 51–60 years, 8 (7.3%) people were operated for cataract.
Educational status
Among the study population, 50 (45.9%) had no formal education, 31 (28.4%) had only primary education, 18 (16.5%) had secondary education, and 10 (9.2%) had tertiary education. More educated people avail themselves for cataract surgery than the uneducated [Table 2].
| Educational status | Males (%) | Females (%) | Total (%) |
|---|---|---|---|
| No Education | 20 (40) | 30 (60) | 50 (45.9) |
| Primary | 18 (58.1) | 13 (41.9) | 31 (28.4) |
| Secondary | 11 (61.1) | 7 (38.9) | 18 (16.5) |
| Tertiary | 6 (60) | 4 (40) | 10 (9.2) |
| Total | 55 (50.5) | 54 (49.5) | 109 (100) |
Original
While more educated men were operated, fewer educated women were operated. This was, however, not statistically significant (P > 0.5).
Systemic comorbidities
26 patients had diabetes only and 30 hypertension only, while ten were both hypertensive and diabetic.
Pre-operative VA
Pre-operative VA showed 44(40.4%) had perception of light, 31 (28.4%) with hand motion (HM), and 34 (31.2%) with counting fingers.
Duration of lost vision before cataract surgery
This study revealed that 67 (61.5%) had lost vision in index eye more than 1 year before presentation for surgery, 34 (31.2%) for 6 months while in 8 (7.3%) people vision loss was for only 3 months. Majority of people with cataract in this part of the world present late for surgery and this can contribute to poor outcome of surgery [Figure 1].

- Duration of delay before surgery. Original
Reasons for delay in surgery
Some of the reasons given in the study for delay in cataract surgery include [Figure 2]:
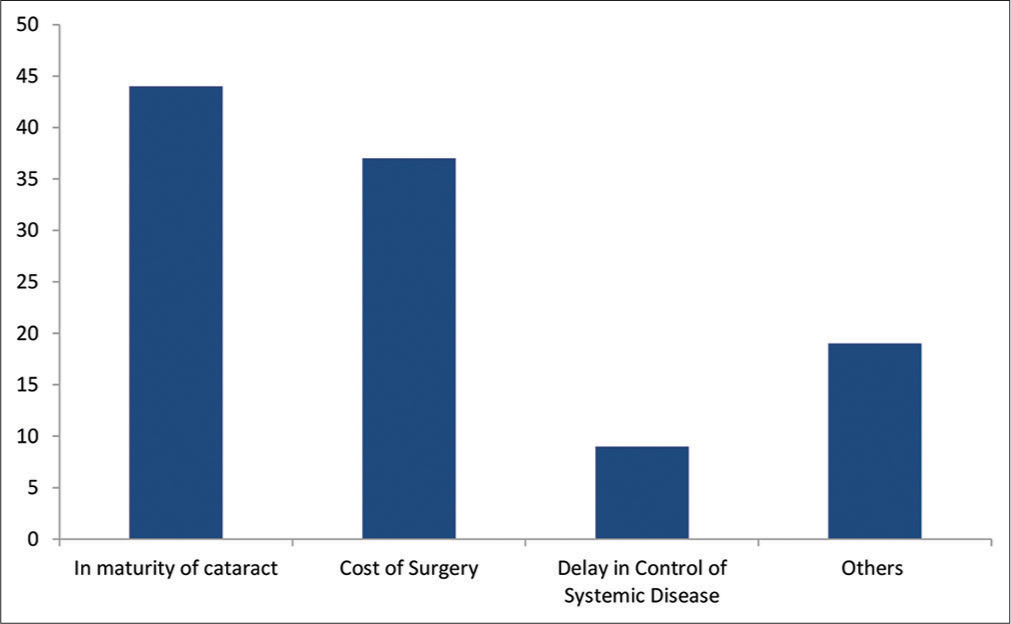
- Reasons for delay in cataract surgery. Original
Immaturity of cataract 44 (40.4%), cost of surgery 37 (33.9%), and delay in control of systemic diseases 9 (8.3%). Other reasons such as poor outcome of cataract surgery, lack of accompanying person, distance from hospital, and not knowing surgery can restore vision 19 (17.4%) were also given.
Visual outcome
First day post-operative unaided VA revealed 31 (28.4%) had 6/6–6/18, 65 (59.6%) with <6/18–6/60, and 13 (12.0%) had <6/60. Pin hole VA was not assessed due to inconsistency in the result.
One-week post-operative number of people with good vision (VA 6/6–18) improved to 46 (42.2%), those with border line (VA<6/18–6/60) improve to 50 (45.9%) while 13 (11.9%) had poor vision (<6/60). VA with Pinhole further improved the number of people with good vision (6/6–6/18) to 54 (49.5%), while people with borderline vision (<6/18–6/60) decreased to 45 (41.3%) and those with poor vision (<6/60) also decrease to 10 (9.2%).
Two months post-operative showed further improvement in number of those with unaided good vision (6/6–6/18) to 65 (59.6%) while 35 (32.1%) had borderline (<6/18–6/60) and 9 (8.3%) with poor vision (<6/60). After refraction, 82 people (75.2%) had improved VA to 6/6–6/18, 21 (19.3%) had <6/18–6/60 while 6 (5.5%) remain at <6/60. Figure comparing VA before surgery and VA after surgery can be seen below [Table 3].
| Category of Vision | Pre-op | 2 months post-op | ||
|---|---|---|---|---|
| Unaided | Aided | Unaided | Aided | |
| PL | 44 | 44 | 0 | 0 |
| HM | 31 | 31 | 0 | 0 |
| <6/60<3/60 | 34 | 34 | 9 | 6 |
| <6/18–6/60 | 0 | 0 | 35 | 21 |
| 6/6–6/18 | 0 | 0 | 65 | 82 |
| Total | 109 | 109 | ||
Original
Complications
Twenty-six patients (24.5%) had surgical complications. Among those with complications 6 (23.1%) had intra-operative posterior capsular (PC) rent with vitreous loss, 2 (7.7%) had iris tear, and 3 (11.5%) had hyphaema, while early post-operative complications include; 9 (34.6%) had corneal edema, 3 (11.5%) cortical remnants, 2 (7.7%) uveitis, and 1 (3.9%) with endophthalmitis.
IOL power used
PCIOL used ranged from 19.00 to 21.00 diopter sphere (Ds) while ACIOL available was 17.50 to 18.00 Ds and powers were selected based on subjective assessment of the eyes as stated earlier. The ACIOL power requirement is normally 2.00 Ds less than an equivalent PCIOL. This is to account for the difference in distance between the ACs and the posterior capsule.
DISCUSSION
Age and sex distribution
The study population consisted of people in the age range of 40–80 years with mean age of 66 years. This age range is similar to the age of cataract patients in other studies in Nigeria[10-15] and elsewhere.[18,19]
There was a marginal male preponderance in this study as in a similar study[15] in the northern senatorial zone of same state as against a wider difference between male and females in other studies.[11,12,14]
The reason for this marginal difference in this study is not known but it can be suggested that the surgery was done at a period of early harvest of crops and most men might have been busy at their farms.
Pre-operative VA
The PVA in this study was poor (VA <6/60) which is similar to other studies within Kaduna State and elsewhere in Nigeria.[13,15] This is because most patients in these studies are rural farmers and petty traders whose visual demands are less than those of skilled workers in urban setting[4] hence they present only when vision is poor. In Europe and other developed countries patients present early for surgery with better VA because of higher visual demands.[4] Late presentation in our study and Africa generally may also be associated with poverty, illiteracy, and ignorance of the curative power of cataract surgery.[16]
Post-operative complications
Post-operative complications were 26 (23.9%) which is lower than 32.9% reported in another study in the northern senatorial district of Kaduna state[15] that used ECCE which might account for the disparity. Result of this study was higher than what was reported by other studies[13,20] among Africans. Studies showing higher complications were either done over a period of more than 1 year or as a result of ACIOL use.[15,19] Corneal edema was the most common postoperative complication in this study which is similar to other studies.[13,15] It is a major cause of poor vision during early post-operative period which can be avoided by maintaining adequate AC depth with viscoelastic substances such as viscomet, reduction in AC manipulation, and good patient selection with good surgical skills. Endophthalmitis is a dreaded complication of cataract surgery and only 1 patient had it. Source of infection could not be traced but we suspected poor facial hygiene despite health talk on this issue pre- and post-operative. The patient presented 1 week after surgery and had daily sub-conjunctiva ceftriaxone, 2 hourly ciloxan, dexamethasone, and tropicamide eye drops. The subconjunctiva ceftriaxone was for 72 while patient continued with other eye drops and systemic ciprofloxacin. There was no improvement in visual outcome thereafter. Intravitreal tap for culture and sensitivity along with intravitreal antibiotics was not done because of logistic concerns.
Systemic diseases
This study showed 66 (60.6%) had either hypertension, diabetes or both which is higher than what was found in studies by Nwosu and Onyekwe[10] and Bekibele et al.[11] within Nigeria and Desai et al. in UK.[18] However, in this study, these systemic conditions were well controlled prior to surgery and did not interfere with the surgery or its outcome. Systemic diseases can contribute to pre-existing ocular pathology which is the largest cause of poor outcome after cataract surgery.[17]
Post-operative VA
First day post-operative VA revealed 30 people (27.3%) had good vision (VA of 6/6–6/18), this is higher than results of other studies within Nigeria.[13,15] This disparity could be attributed to the 70% number of patients with corneal edema postoperatively in their studies against the 14.3% recorded in this study. Result from this study is comparable to a large survey in Africa.[16] Number of people with good PVA kept improving from 27.3% of 1st day post-operative through 42.2% in 1 week to 59.6% after 8 weeks. Those with BCVA at 8 weeks increased to 75.6%. Those with good PVA at 8 weeks in this study showed slight improvement over a similar study in Ago-Iwoye south-west Nigeria[13] though VA was checked after 6 weeks against 8 weeks in this study. Results of other studies within Nigeria showed fewer people with good VA.[12,14-16]
A population study across most developed countries has revealed that most operated cases do not achieve the WHO target of visual outcome.[21]
CONCLUSION
Cataract is still a major cause of blindness in Nigeria and MSICS +IOL is very effective in managing cataract backlog. Poor visual outcome may be caused by surgical complications, absence of technological support, for example, biometry, slit lamp for pre-operative preparation of patient and follow-up. There is need for surgeons and supporting staff to audit their performance regularly to meet the expectation of patients. Although people with good visual outcome in this study were less than the WHO requirement, it forms a good basis for future improvement in visual outcome of cataract surgery.
Recommendation
Biometric assessment of the eye for objective choice of IOL along with provision of portable slit lamp for adequate pre-operative assessment and follow-up couple with improvement in surgical skills and newer surgical methods like Phacoemulsification can improve visual outcome to the expected WHO recommendation and beyond.
Acknowledgment
I wish to appreciate the management of Sir Ibrahim Patrick Yakowa General Hospital, Kafanchan and Staff of the eye unit for their invaluable support during the study period.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Review of publications of the Nigeria national blindness survey: Methodology, prevalence, causes of blindness and visual impairment and outcome of cataract surgery. Ann Afr Med. 2012;11:125-30.
- [CrossRef] [PubMed] [Google Scholar]
- Fact Sheet No. 282. Available from: http://www.who.int/mediacentre/factsheets/fs282/en/index.html [Last accessed 2022 Jan 28]
- [Google Scholar]
- Outcome of cataract surgery from outreach eye camp. Delhi J Ophthalmol. 2014;25:90-4.
- [CrossRef] [Google Scholar]
- Cataract-a global perspective: Output, outcome and outlay. Eye. 1999;13:449-53.
- [CrossRef] [PubMed] [Google Scholar]
- Eye care outreach to rural underserved population in Edo and Delta States of Nigeria. JMBR. 2004;3:83-90.
- [Google Scholar]
- Visual Function and quality of life among cataract operated and unoperated blind population in Nepal. Br J Ophthalmol. 1998;82:606-10.
- [CrossRef] [PubMed] [Google Scholar]
- Visual acuity and quality of life in patient with cataract in Doumen country, Guanzhou Province, China. Ophthalmology. 1999;106:1609-15.
- [CrossRef] [Google Scholar]
- Population based assessment of the outcome of cataract surgery in an urban population in Southern India. Am J. Ophthalmol. 1999;127:659-65.
- [CrossRef] [Google Scholar]
- Informal Consultation on Analysis of Blindness Prevention Outcomes, WHO/PBL/98/68 Geneva: World Health Organization; 1998.
- [Google Scholar]
- Intraocular lens implant surgery in Onitsha Nigeria. Nig J Ophthalmol. 2002;10:5-9.
- [CrossRef] [Google Scholar]
- Evaluation of the outcome of ECCE surgery wih PCIOL at Ago-Iwoye, Ogun state Nigeria. Nig J Ophthalmol. 2001;9:32-6.
- [CrossRef] [Google Scholar]
- Assessment of one year follow-up of patients with ECCE PCIOL surgery at university of Ilorin teaching hospital, Kwara state Nigeria. Nig J Ophthalmol. 2004;12:65-9.
- [CrossRef] [Google Scholar]
- Visual Outcome after small incision cataract surgery in South Western Nigeria. Nig J Ophthalmol. 2010;18:40-4.
- [CrossRef] [Google Scholar]
- Evaluation of cataract surgery outcome in Western Nigeria. Ghana Med J. 2009;43:169-74.
- [Google Scholar]
- Outcome of cataract surgery in rural areas of Kaduna state, Nigeria. Ann Afr Med. 2014;13:23-9.
- [CrossRef] [PubMed] [Google Scholar]
- Does prospective monitoring improve cataract surgery outcomes in Africa? Br J Ophthalmol. 2002;86:543-7.
- [CrossRef] [PubMed] [Google Scholar]
- Visual function and post-operative care after cataract surgery in rural China. Arch Ophthalmol. 2007;11:125-7.
- [CrossRef] [PubMed] [Google Scholar]
- Profile of Patients presenting for Cataract Surgery in UK: National data collection. Br J Ophthalmol. 1999;83:893-6.
- [CrossRef] [PubMed] [Google Scholar]
- Is anterior Chamber lens implantation after cataract extraction safe in rural black patients in Africa? A pilot study in Kwazulu-Natal. South Africa. Eye. 1998;12:821-5.
- [CrossRef] [PubMed] [Google Scholar]
- Report from European Cataract outcome study group, 1998 European cataract outcome study. J Cataract Refract Surg. 2001;27:1176-84.
- [CrossRef] [Google Scholar]






