Translate this page into:
Efficacy and safety of pre-operative individual topical mydriatic and anaesthetic versus an intracameral fixed-dose combination of two mydriatics and an anaesthetic for phacoemulsification – A comparative study
*Corresponding author: Kajal Haribhai Kataria, Department of Ophthalmology, M and J Western Regional Institute of Ophthalmology, Ahmedabad, Gujarat, India. kajalkataria1234@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kataria KH, Bhagat PR, Sedani KV, Mehta HN. Efficacy and safety of pre-operative individual topical mydriatic and anaesthetic versus an intracameral fixed-dose combination of two mydriatics and an anaesthetic for phacoemulsification – A comparative study. Glob J Cataract Surg Res Ophthalmol 2022;1:21-5.
Abstract
Objectives:
Intracameral fixed combination of mydriatic and anaesthetic is a new method for inducing and maintaining intraoperative mydriasis and analgesia during cataract surgery. The purpose of our study was to evaluate the efficacy and safety of an intracameral fixed-dose combination of phenylephrine 0.31%, tropicamide 0.02%, and lidocaine 1% during phacoemulsification in comparison to the standard pre-operative topical regimen.
Materials and Methods:
Fifty patients undergoing phacoemulsification were randomly divided into two groups, A and B. Surgery was performed by a single surgeon, using standard regimen in Group A and using the intracameral formulation in Group B. The outcome measures were pupil size, patient perception of pain and overall comfort, surgeon rating of overall experience, and safety.
Results:
Post-dilatation, the pupillary diameter was 7.7 ± 1.3 mm and 5.5 ± 1.2 mm, respectively, for Groups A and B which was statistically significant. For the perception of pain as well as overall comfort, in Group A, five patients rated 4 and 20 patients rated 5, and in Group B, two patients rated 4 and 23 rated 5. The surgeon rating for all patients of Group A was 5 but in Group B, for three patients, it was 4 because of inadequate and ill sustained mydriasis. No complications occurred in either group.
Conclusion:
Intracameral fixed combination of mydriatic and analgesic is safe and effective for use by experienced ophthalmologists and in uncomplicated cataract, providing a reduced pre-operative time; but because of the variable, lesser and ill sustained mydriasis, it may be avoided in complicated cataracts and by novice surgeons.
Keywords
Phacoemulsification
Topical anaesthesia
Intracameral anaesthesia
INTRODUCTION
A cataract is the leading cause of preventable blindness in the world and cataract extraction with intraocular lens (IOL) implantation is perhaps the most effective surgical procedure in all of medicine.[1] Cataract surgery also constitutes by far the most common surgical procedure performed under local anaesthesia. Thus, it is necessary that the anaesthesia for cataract surgery be equally safe. Retrobulbar anaesthesia (RBA) was previously commonly used for cataract extraction. Due to the serious needle-related complications associated with RBA such as retrobulbar haemorrhage, optic nerve damage, and globe perforation,[2] it was gradually replaced by peribulbar anaesthesia (PBA) (using 2% lignocaine and 0.5% bupivacaine in a ratio of 2:1 with hyaluronidase 5 IU/ml and adrenaline one in 1 lac). PBA is considered by many as the conventional mode of anaesthesia for cataract surgery due to its advantages of adequate globe anaesthesia and akinesia. Its disadvantages include delayed visual recovery, risk of post-operative ptosis, and occasional sight-threatening complications such as globe perforation and optic nerve damage. In modern-day technologically advanced microincisional cataract surgery, therefore, PBA has been replaced by other less invasive modes of anaesthesia such as sub-Tenon’s, topical and intracameral. Patients too are becoming increasingly aware and expect and demand better surgical and post-surgical comfort as well as early visual recovery. Such newer methods of anaesthesia have advantages such as reduced surgical time, early postoperative recovery, and freedom from hospitalisation. The disadvantages of using pre-operative topical mydriatic and an anaesthetic are repeated instillations before surgery to ensure adequate intraoperative mydriasis and analgesia, probability of ocular surface toxicity, and risk of wash out from multiple drug instillations. With the launch of intracameral fixed-dose combination (FDC) of mydriatics and anaesthesia, their major advantages reported in comparison with the topical regimen are single use, no ocular surface toxicity, and decreased incidence of cardiovascular side effects.[3] Intracameral mydriatic and anaesthetic are efficient and safe method for inducing and maintaining intraoperative mydriasis and analgesia, leading to increased patient comfort (especially during IOL implantation) and surgeon satisfaction.[4,5] However, this being a relatively newer modality, not much safety and efficacy data exist in the literature, especially in the Indian subpopulation. Therefore, through this study, we have investigated the efficacy and safety of intracameral FDC of phenylephrine 0.31%, tropicamide 0.02%, and lidocaine 1% during phacoemulsification in comparison to conventionally used pre-operative individual topical mydriatic (tropicamide 0.8%and phenylephrine 5%) and anaesthetic drug (proparacaine hydrochloride 0.5%).
MATERIALS AND METHODS
This prospective, randomised, comparative, interventional study was conducted from February 2021 to July 2021, among patients attending our tertiary healthcare referral centre, diagnosed to have immature senile cataract (age 50– 70 years) with adequate pre-operative pupillary dilatation (≥6 mm) and scheduled to undergo cataract surgery. Patients with cataract due to reasons other than ageing, having ocular and/or systemic pathologies, using drugs likely to influence pupillary dilatation and iris tissue response (e.g., tamsulosin), having gross corneal abnormalities as evident on slit-lamp examination, unable to understand verbal commands, with known sensitivity to lidocaine, with significant anxiety, with unintentional eye movements and who did not give consent were excluded from the study. Ethical clearance for the study was obtained from our Institutional Ethics Committee. Informed consent was obtained from every subject after explaining the procedure, before their enrolment into the study.
A total of 50 patients were enrolled and divided into two groups, A and B. Patients were alternately randomised to Group B. All patients underwent routine pre-operative cataract surgery assessment and investigations. On the day of surgery, patients in Group A (n = 25) were administered one drop of topical mydriatic agent (tropicamide 0.8% with phenylephrine 5%) in the eye to be operated, starting 30 min before surgery and instilled 10 min apart, as per the traditional protocol and one drop of topical anaesthesia (proparacaine hydrochloride 0.5%) at 5 min interval, started 15 min before surgery. Patients in Group B (n = 25) were operated using 0.1 ml intracameral FDC of phenylephrine 0.31%, tropicamide 0.02%, and lidocaine 1% without the use of any pre-operative drops. The pupil diameter of the eye to be operated on was measured by the operating surgeon under the microscope using a surgical Castroviejo calliper at two specific time points (T0 and T1). For Group A, T0 was measured before initiation of administration of topical mydriatic agents and T1 10 min after the third instillation of the topical mydriatic agent. For Group B, T0 and T1 were measured immediately before and after the injection of the intracameral formulation, respectively. Preoperatively, all patients were counselled on the potential intraoperative visual experience, namely light perception, fingers, instruments, and the gush of fluid.[6,7] All patients were operated on by a single surgeon following aseptic precautions as per the institutional protocol. Patients were instructed to keep their sight fixed on the light of the operating microscope throughout the procedure. All the surgeries were performed by the phacoemulsification direct chop technique, with posterior chamber in-the-bag IOL implantation, using machine parameters as necessary for the procedure. No drugs likely to influence pupil size were used (in the irrigating fluid or intracamerally) during the surgery. A drop of moxifloxacin 0.5% as an antibiotic was instilled on the ocular surface at the end of the surgery. After completion of the surgery, each patient was asked to rate the level of pain felt during the surgery (as per the visual analogue scale: No pain, mild pain, and moderate pain)[8] and also rate the overall comfort during surgery on a scale of 0–5 (0 = extremely uncomfortable and 5 = very comfortable). The surgeon was also asked to rate the comfort during surgery on a scale of 0–5 (0 = extremely uncomfortable and 5 = very comfortable). All the patients were initiated on topical moxifloxacin eye drops 0.5% gel formulation twice a day and prednisolone eye drops 1% 2 hourly in the operated eye. The follow-up examinations were scheduled on day 1 and day 7 postoperatively for visual acuity assessment and slit-lamp biomicroscopy.
The data collected from the patients and surgeons were analysed using Microsoft Excel. Frequency and percentages were calculated and P-value derived using Chi-square test. P < 0.05 was considered statistically significant.
RESULTS
A deepened analysis comparing characteristics of all the patients in two different groups is summarised in [Table 1]. Considering the mean pupil diameter at T1 that is, 7.7 ± 1.3 mm and 5.5 ± 1.2 mm in Groups A and B, respectively, the difference in pupil sizes was found to be statistically significant (P < 0.000).
| Variable | Group-A (individual topical mydriatic and anaesthetic drug) | Group-B (intracameral fixed-dose combination of mydriatic and anaesthetic) |
|---|---|---|
| Age | 50–60 years: 18 (36%) patients | 50–60 years: 13 (26%) patients |
| 61–70 years: 7 (14%) patients | 61–70 years: 12 (24%) patients | |
| Gender | Male: 14 (28%) patients | Male: 15 (30%) patients |
| Female: 11 (22%) patients | Female: 10 (20%) patients | |
| Pre-operative binocular corrected visual acuity (as on Snellen chart) | <6/36: 9 (18%) patients | <6/36: 7 (14%) patients |
| 6/36 to 6/6: 16 (32%) patients | 6/36 to 6/6: 18 (36%) patients | |
| Mean pre-operative preparation time | 37.5±7.5 min | 7.5±2.5 min |
| Mean pupillary diameter | ||
| T0 | 1.7±0.5 mm | 1.5±0.5 mm |
| T1 | 7.7±1.3 mm | 5.5±1.2 mm |
| Mean surgical time | 21.12±2 min | 21.24±3 min |
| Complications | Mild ocular hyperaemia: 1 (4%) patient, only at day 1 | Mild ocular hyperaemia: 1 (4%) patient, only at day 1 |
Postoperatively on day 1 and on day 7, slit-lamp biomicroscopic examination in both groups showed no untoward findings such as significant cells, flare, corneal oedema, or complications. Mild hyperaemia was noted in both groups in just one patient each, on the 1st operative day, which was insignificant.
The patient rating for pain as per the visual analogue scale and overall comfort is depicted in [Figures 1 and 2], respectively. Surgeon rating for overall comfort during surgery is shown in [Figure 3]. In Group B, for three cases, the surgeon rated 4 because of a qualitative experience of inadequate and ill sustained mydriasis during different steps of the surgery in different patients.
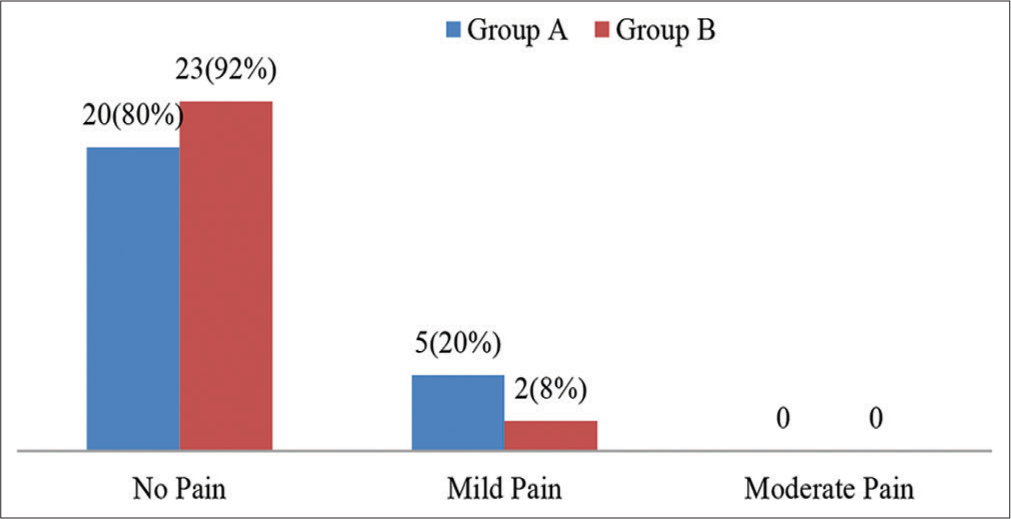
- Patient rating for pain according to visual analogue scale in Group A and Group B.

- Patient rating for overall comfort during surgery in Group A and Group B.

- Surgeon rating for overall comfort during surgery for Group A and Group B.
DISCUSSION
Optimal mydriasis and anaesthesia are the key factors influencing the safety of cataract surgery and the patient’s comfort in the perioperative period. Due to its quicker onset of anaesthesia, better consistency, effectiveness, and better patient compliance as well as faster post-operative patient rehabilitation, topical anaesthesia is slowly replacing the use of the peribulbar block. However, patients do experience some intraoperative pain, especially during iris tissue contact or manipulation.[8] Intracameral anaesthesia is a newer option providing a dual and simultaneous benefit of mydriasis and analgesia in modern cataract surgery. Surgeons may also use intracameral anaesthesia for incremental pain control in patients who cannot be adequately managed with topical anaesthesia alone and for the need of added intraoperative mydriasis. However, an intracameral combination of an anaesthetic and mydriatic is not as effective in providing mydriasis as its topical counterpart as seen in our study wherein in Group A, the mean pupillary diameter at T1 was 7.7 ± 1.3 mm, whereas, in Group B, it was 5.5 ± 1.2 mm. A study was done by Labetoulle et al.[4] reported that mean pupil size in the Mydrane (phenylephrine 0.31%, tropicamide 0.02%, and lidocaine 1%) group was approximately 7.5 mm. Another study was done by Gupta et al.[9] who reported a mean pupil size of 7 mm in the intracameral mydriatic drug (lignocaine 0.75–1% with epinephrine 0.025%).
In our study, the mean pre-operative preparation time in Group A was 37.5 ± 7.5 min and in Group B was 7.5 ± 2.5 min. Thus, pre-operative time was much lower in the intracameral group as there was no requirement for instillation of topical drops. A reduction in time spent in the pre-operative room can lead to a less stressful experience for patients and shorter hospital stay. Findings in our study were similar to the study done by Labetoulle et al.[4] and Nuzzi et al.[10] The average surgical time was similar between groups in our study and was comparable to the findings of Labetoulle et al.[4]
In our study, 80% of patients in Group A and 92% of patients in Group B did not complain of any pain while 20% of patients in Group A and 8% of patients in Group B experienced mild pain according to the visual analogue scale. A study was done by Shakya et al.[8] who reported that 30% of patients in Group A (topical anaesthesia with proparacaine hydrochloride 0.5%) and 80% of patients in Group B (topical anaesthesia with intracameral infiltration 0.5 cc of 1% lidocaine) had no pain, while 50% of patients in Group A and 20% of patients in Group B had mild pain according to the same scale.
In our study, just one patient in each group developed mild ocular hyperaemia on day 1. The study was done by Labetoulle et al.[4] who reported that 19.1% of patients in the reference group (tropicamide 0.5% and phenylephrine 10%) and 17.7% in the Mydrane group (intracameral fixed combination of phenylephrine 0.31%, tropicamide 0.02%, and lidocaine 1%) developed complications such as mild ocular oedema and hyperaemia, moderate macular oedema, mild-to-severe keratitis, increased intraocular pressure and posterior capsule rupture. The concentration of the constituents in the intracameral group was low compared with topical mydriatic, which should perhaps ensure greater safety and lower incidence of side effects.
A greater proportion of our patients (92%) showed better comfort in Group B compared to Group A (80%). However, the surgeon’s comfort during surgery was better in Group A (100%) compared to Group B (88%) probably due to the adequate and sustained dilatation being maintained in Group A.
A limitation of the study was that the effect of the new FDC on the IOP and corneal endothelium through specular microscopy was not done. A continued study on more patients can perhaps help to study the results of ill sustained pupil dilatation in some patients of Group B. Nevertheless, a totally normal slit-lamp biomicroscopic examination in both groups in the post-operative period rules out any significant effects.
CONCLUSION
Intracameral fixed combination of phenylephrine 0.31%, tropicamide 0.02%, and lidocaine 1% is a new, feasible alternative to the use of topical drugs. It has been found to be effective and safe in providing adequate anaesthesia, analgesia, and mydriasis during routine uncomplicated phacoemulsification for an experienced ophthalmologist with a reduced pre-operative time. However, because of the variable, lesser, and ill sustained mydriasis, it may be avoided in hard and/or complicated cataracts. It may also be avoided by novice surgeons due to the same reason. This technique is not inferior when compared to the traditional use of individual topical anaesthesia and mydriatic agents in providing adequate patient comfort and surgeon ease.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Comparison of subtenon anesthesia with peribulbar anesthesia for manual small incision cataract surgery. Indian J Ophthalmol. 2005;53:255-9.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of peribulbar anesthesia with sub-tenon's in manual small incision cataract surgery. TNOA J Ophthalmic Sci Res. 2018;56:67-70.
- [CrossRef] [Google Scholar]
- Intracameral mydriatics in phacoemulsification cataract surgery. J Cataract Refract Surg. 2003;29:2366-71.
- [CrossRef] [Google Scholar]
- Evaluation of the efficacy and safety of a standardized intracameral combination of mydriatics and anesthetics for cataract surgery. Br J Ophthalmol. 2016;100:976-85.
- [CrossRef] [PubMed] [Google Scholar]
- Phacoemulsification under topical anesthesia alone versus topical anesthesia with intracameral lidocaine injection. IOSR J Dent Med Sci. 2012;3:8-12.
- [CrossRef] [Google Scholar]
- Patients' visual experience during phacoemulsification cataract surgery and associated fear. BMC Res Notes. 2014;20:663.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of preoperative counseling on fear from visual sensations during phacoemulsification under topical anesthesia. J Cataract Refract Surg. 2011;37:814-8.
- [CrossRef] [PubMed] [Google Scholar]
- Topical proparacaine vs combined topical-intracameral lidocaine anesthesia in phacoemulsification surgery with preoperative counseling about intraoperative visual fear. J Adv Acad Res. 2018;4:82-8.
- [CrossRef] [Google Scholar]
- Phacoemulsification without preoperative topical mydriatics: Induction and sustainability of mydriasis with intracameral mydriatic solution. Indian J Ophthalmol. 2014;62:333-6.
- [CrossRef] [PubMed] [Google Scholar]
- Efficacy and safety of an intracameral combination of two mydriatics and an anesthetic for phacoemulsification in complicated patients. Open Ophthalmol J. 2018;12:322-9.
- [CrossRef] [Google Scholar]






