Translate this page into:
Is opposite clear cornea incision useful still? – A tertiary institute experience
*Corresponding author: Yong Wei Wei Dayna, Department of Ophthalmology, National University Hospital, Singapore. daynayong6@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tan Y, Dayna YWW, Shen L, Chew GW, Chen J. Is opposite clear cornea incision useful still? – A tertiary institute experience. Glob J Cataract Surg Res Ophthalmol. 2024;3:71-4. doi: 10.25259/GJCSRO_9_2024
Abstract
Objectives:
Paired opposite clear corneal incision (OCCI), placed at the steepest meridian, during phacoemulsification cataract surgery is one of the options used to improve pre-existing astigmatism, which enhances the flattening effect. Our surgical technique for OCCI consists of a 2.75-mm stab clear corneal incision with a steel microkeratome. In this series, we retrospectively review the effect of OCCI on reducing preoperative corneal astigmatism done by a single surgeon.
Materials and Methods:
From October 2021 to May 2022, 53 eyes underwent phacoemulsification cataract surgery with OCCI. All eyes completed refractive analysis at least at postoperative month 1.
Results:
There were 22 males (45.1%) and overall mean age was 70.8years. Mean corneal astigmatism preoperatively was -1.98±0.57D. At postoperative month 1, the mean change in spherical equivalence was 0.97 ± 2.8D (P = 0.37). The mean reduction in corneal astigmatism was 1.07±0.83D (P <.001). At postoperative month 6 (n = 17), mean reduction in corneal astigmatism compared to preoperatively was 0.89±0.74D (P = <0.001). Mean corneal astigmatism increased between postoperative month 1 and month 6 at 0.15 ± 0.79D but this was not statistically significant. Age was not found to be correlated to change in astigmatism (r = 0.156).
Conclusion:
Paired OCCI is a useful technique to correct pre-existing astigmatism with no additional need to alter surgical setting.
Keywords
Corneal procedures for astigmatism <refractive surgery
Phacoemulsification <lens/cataract
Refractive surgery
Lens/cataract
Surgical instruments/special techniques <lens/cataract
INTRODUCTION
Astigmatism is a common refractive error worldwide, affecting approximately 60% of Singaporeans over the age of 40.[1] Over 80% of patients undergoing cataract surgery have some degree of cornea astigmatism, and around 30% have more than −1.5D of corneal astigmatism.[2] Following cataract surgery, corneal astigmatism will persist and can impact a patient’s quality of life.
The ideal treatment for such patients would be the implantation of toric intraocular lenses (IOLs). However, these cost more and have up to 20% risk of rotating postoperatively, which might necessitate a second surgery.[3] Patients unable to afford toric IOLs or unwilling to accept the potential need for a second surgery will have to live with potentially significant degrees of post-operative astigmatism.
Non-toric options to treat corneal astigmatism are well described, and these include making the main port incision at the steepest corneal axis or using spectacles or contact lenses postoperatively. Surgically induced astigmatism is known to occur during clear corneal incision phacoemulsification cataract surgery as a result of flattening of the cornea, but this effect can be used to benefit patients with pre-existing astigmatism.[4] The goal of surgery is to restore vision to the patient in the least complicated manner, and correction of pre-existing astigmatism through opposite clear corneal incisions (OCCIs) in cataract surgery can be done so without any additional skills or instruments.[5] Through exploring the safety and efficacy of OCCIs, an old and less popularised technique, we evaluate this alternative treatment for patients seeking non-toric lens options.
In a local context, literature has been published regarding clear corneal incision and some of its risks but the use of OCCI to treat pre-existing astigmatism is not as well explored. OCCI has been shown to be a reliable method of correcting mild astigmatism.[6] Even though OCCI is a relatively simple technique requiring no extra instrumentation and can be done in routine settings, it is not done commonly due to drawbacks such as difficulty with certain axes. Techniques differ among surgeons with variations in the length of incision, distance from limbus, paired or unpaired and threshold for OCCI. This study aims to examine the utility of OCCI as a cheap, quick and safe way of reducing postoperative astigmatism in patients who decline toric IOLs.
MATERIALS AND METHODS
This is a retrospective analysis of patients operated on by a single surgeon. Data was collected from the hospital’s electronic medical records. Between 1 October 2021 and 31 May 2022, patients who underwent uncomplicated phacoemulsification cataract surgery, had non-toric mono-focal IOLs implanted and had an OCCI were included in this study. Preoperatively, routine eye examinations were conducted in the clinic, including refraction, slit-lamp examination and dilated fundoscopy. Biometry was calculated using both IOLMaster 500 and 700 models. The National Healthcare Group Domain Specific Review Board approved this study.
A single-plane main port incision was created at the steepest meridian (determined by IOLMaster and Auto-keratometry readings) with a 2.75 mm microkeratome blade. Standard phacoemulsification was performed. An OCCI was performed after the IOL was implanted before removing the viscoelastic. No wounds were extended. All IOLs were implanted in the capsular bag.
Pre-operative and post-operative parameters taken into consideration included mean axial length, mean corneal astigmatism and keratometry in 2 meridians (flat keratometry K1 and steep keratometry K2).
Statistical analysis was performed using the Statistical Package for the Social Sciences Version 29.0 software (IBM Corporation, Armonk, NY, USA). P < 0.05 were considered statistically significant.
RESULTS
In total, 53 eyes underwent phacoemulsification cataract surgery with OCCI. All intraocular lenses were implanted in the capsular bag with no post-operative complications noted. All patients completed refractive analysis for at least 1 month postoperatively. Among the 53 patients included in this study, 22 (45.1%) were male, and 23 were female (54.9%), with a mean age of 70.8 years. The youngest participant was 36 years old, and the oldest was 93 years old.
The mean axial length, as measured preoperatively, was 24.09 ± 1.23 mm. Mean corneal astigmatism was calculated to be −1.98 ± 0.57 D. Mean keratometry findings were 43.46 ± 1.62 D for K1 and 45.44 ± 1.71 D for K2. Only three types of IOL were implanted in our study, with a distribution of 45 (84.9%) using the SA60AT model, 6 (11.3%) using the AAB00 model and 2 (3.8%) using the AR40E model. The mean IOL power was calculated to be 17.79 ± 4.18 D. The pre-operative findings are summarised in Table 1.
| Characteristics | n=53 |
|---|---|
| Male (%) | 22 (45.1) |
| Mean age (range) | 70.8 (36–93) years |
| Mean axial length (SD) | 24.09±1.23 mm |
| Mean corneal astigmatism (SD) | −1.98±0.57 D |
| K1 | 43.46±1.62 D |
| K2 | 45.44±1.71 D |
| IOL implanted (%) | |
| SA60AT | 45 (84.9) |
| AAB00 | 6 (11.3) |
| AR40E | 2 (3.8) |
| Mean IOL power | 17.79±4.18 D |
IOL: Intraocular lens, SD: standard deviation, D: Dioptre
There were no incision-related complications detected on subsequent follow-up visits including wound leakage or endophthalmitis. Patients were subsequently followed up for 6 months postoperatively, and the findings on clinical examinations at 1 month and 6 months are presented in Figure 1a and b. Figure 1a compares the pre-operative and post-operative months’ 95% confidence interval for corneal astigmatism. Mean astigmatism at post-operative month 1 was −1.11D, and at month 6 was −1.26D. There was an improvement in corneal astigmatism at postoperative month 1 and no rebound in corneal astigmatism at postoperative month 6.
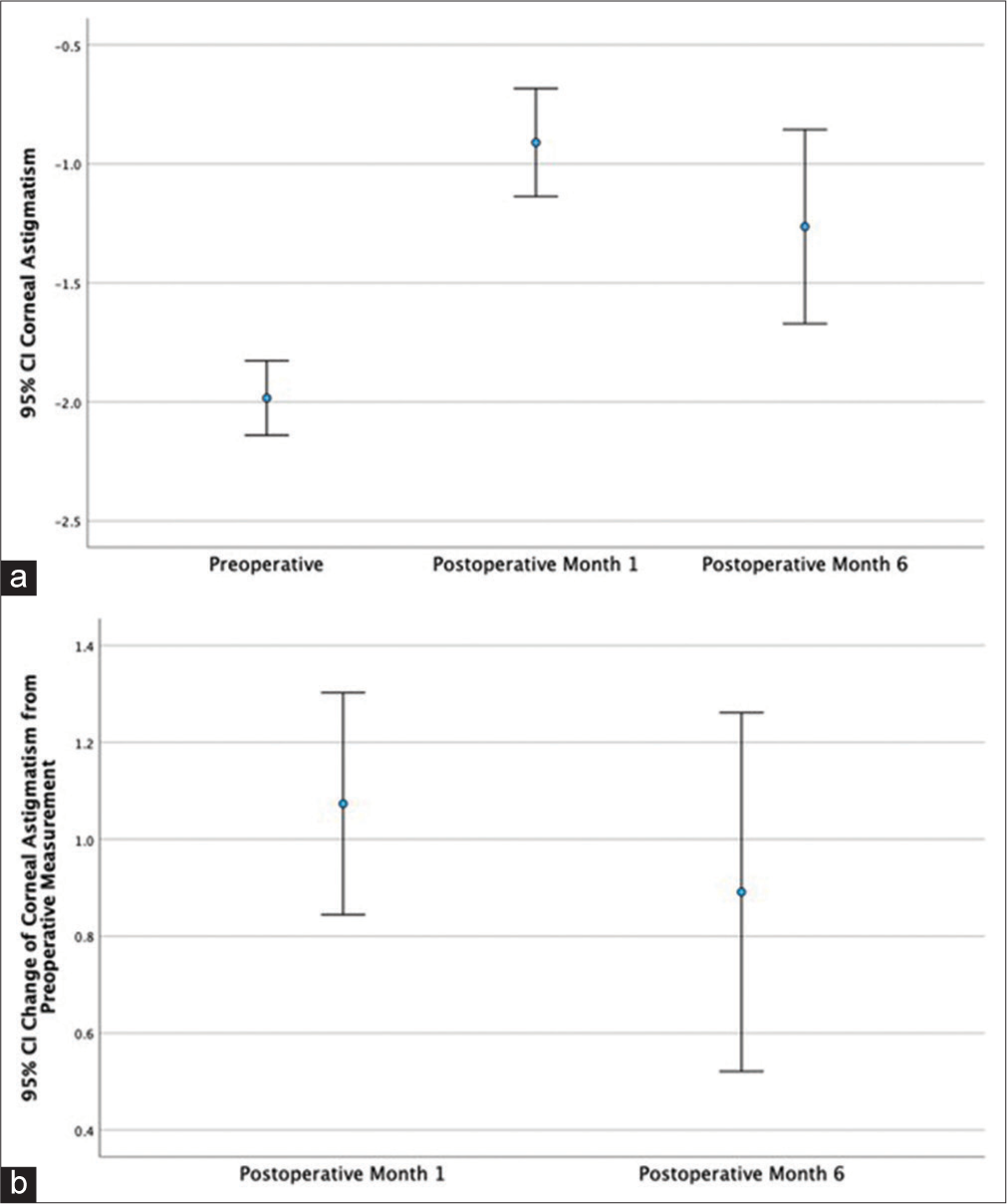
- (a) Figure comparing the pre-operative and post-operative months’ 95% confidence interval for corneal astigmatism. (b) Figure showcasing the change of 95% confidence interval of corneal astigmatism from pre-operative measurement at postoperative months 1 and 6, CI= Confidence interval.
Figure 1b demonstrates the degree of change of corneal astigmatism during the follow-up evaluations at postoperative months 1 and 6. At postoperative month 1 (n = 53), the mean change in spherical equivalence was 0.97 ± 2.80D (P = 0.37), and the mean reduction in corneal astigmatism was 1.07 ± 0.83D (P < 0.001). At postoperative month 6 (n = 17), the mean reduction in corneal astigmatism compared to preoperatively was 0.89 ± 0.74D (P < 0.001). Mean corneal astigmatism increased between postoperative month 1 and month 6 at 0.15 ± 0.79D (P = 0.424), but this was not statistically significant. Age was not found to be correlated to a change in astigmatism (r = 0.156).
DISCUSSION
The post-operative outcomes with respect to corneal astigmatism were within the expected range. Existing literature has recorded a post-operative improvement of corneal astigmatism by 1.23 ± 0.49 diopters in a similar study analysing paired OCCI for pre-existing astigmatism patients,[7] as well as 1.07 ± 0.27 D for paired OCCI in another paper comparing paired OCCI and single clear corneal incision (CCI).[8] Slight variations may be explained due to the varying timeframes that the measurements were taken. Our study analysed patients at postoperative 1 month and 6 months, whereas the two papers mentioned above measured post-operative corneal astigmatism at postoperative 3 months and 12 weeks, respectively. However, this variation is not expected to affect the validity of our post-operative corneal astigmatism readings since the variation between the readings we obtained at 1 month and 6 months was deemed not to be statistically significant. The use of paired OCCI to improve outcomes for patients with pre-existing astigmatism undergoing cataract surgery relies on the principle of inducing a degree of astigmatism to counter the existing corneal defect. This form of surgically induced astigmatism was deemed to be stable both statistically and clinically between 2 weeks and 9 weeks after surgery.[6] Another explanation for the variation could be the difference between with the rule (WTR) and against the rule astigmatism, as WTR astigmatism patients who underwent paired OCCI saw a greater degree of corneal astigmatism correction and were associated with a more stable change postoperatively when compared between 1 and 6 months.[9] Paired OCCI methods vary depending on the incision location and wound length, with a larger incision, typically 3.0 mm or more, inducing a significantly larger degree of astigmatism than microincisional cataract surgery.[6]
Clear corneal incisions help reduce cylindrical power by inducing a flattening of the cornea. The most obvious benefit would be that it does not need any extra equipment or additional technical skills, allowing for the simultaneous management of cataracts and astigmatism. Our data are corroborated with previous studies to show that mild-to-moderate degree of astigmatism can be corrected at negligible extra cost during cataract surgery through the use of the paired OCCI technique.[7] That being said, there are still several limitations that the paired OCCI technique may have. There can be an increased risk of endophthalmitis compared to single clear corneal incisions or non-penetrating procedures. Practical constraints may render surgeons unable to adjust phacoemulsification sites according to the individual patient’s astigmatic axis to perform a paired OCCI since it is an on-axis surgery, and the usage of microincision cataract surgery would make paired OCCI unfeasible as a tool for correcting astigmatism since the small incision does not flatten the cornea sufficiently to induce the necessary astigmatism correction.[7]
There exist situations where paired OCCI would not be best suited for the patient, be it due to high astigmatism that exceeds the range of surgically induced astigmatism potential or the presence of mechanical instabilities in the patient’s anatomy. If OCCI is unsuitable, the authors would suggest using spectacles or contact lenses postoperatively. Toric IOL implantation has been shown to achieve better clinical post-operative outcomes when compared to paired OCCI at the cost of requiring a more expensive lens, which has its own set of potential disadvantages.[7,10] Nevertheless, this study demonstrates that paired OCCI provides a safe and reliable alternative for patients with pre-operative astigmatism undergoing cataract surgery without implantation of a toric lens.
CONCLUSION
Paired OCCI is a useful technique to correct pre-existing astigmatism with no additional need to alter surgical settings.
Ethical approval
The research/study was approved by the Institutional Review Board at NHG DSRB, number 2022/00889, dated 11 April 2023.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Conflicts of Interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Prevalence of refractive errors in a multiethnic Asian population: The Singapore epidemiology of eye disease study. Invest Ophthalmol Vis Sci. 2013;54:2590-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of corneal astigmatism before cataract surgery. J Cataract Refract Surg. 2009;35:70-5.
- [CrossRef] [PubMed] [Google Scholar]
- Toric intraocular lenses: Historical overview, patient selection, IOL calculation, surgical techniques, clinical outcomes, and complications. J Cataract Refract Surg. 2013;39:624-37.
- [CrossRef] [PubMed] [Google Scholar]
- Opposite clear corneal incisions to correct pre-existing astigmatism in cataract surgery. J Cataract Refract Surg. 2000;26:803-5.
- [CrossRef] [PubMed] [Google Scholar]
- Opposite clear corneal incisions versus steep meridian incision phacoemulsification for correction of pre-existing astigmatism. J Ophthalmic Vis Res. 2008;3:87-90.
- [Google Scholar]
- Paired opposite clear corneal incision: Time-related changes of its effect and factors on which those changes depend. Eur J Ophthalmol. 2014;24:676-81.
- [CrossRef] [PubMed] [Google Scholar]
- Paired opposite clear corneal incisions to correct preexisting astigmatism in cataract patients. J Cataract Refract Surg. 2005;31:1167-70.
- [CrossRef] [PubMed] [Google Scholar]
- Corneal astigmatism change and wavefront aberration evaluation after cataract surgery: 'Single' versus 'paired opposite' clear corneal incisions. Adv Biomed Res. 2014;3:163.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of paired opposite clear corneal incisions on with-the-rule versus against-the-rule astigmatism. Cornea. 2015;34:901-5.
- [CrossRef] [PubMed] [Google Scholar]
- Toric intraocular lens versus opposite clear corneal incisions to correct astigmatism in eyes having cataract surgery. J Cataract Refract Surg. 2009;35:451-8.
- [CrossRef] [PubMed] [Google Scholar]







