Translate this page into:
Client’s pre-operative expectations and outcome of cataract surgery at the Jos University Teaching Hospital, Jos, Plateau State, Nigeria
*Corresponding author: Noah Emmanuel Akpa, Consultant Ophthalmologist, Department of Ophthalmology, Dalhatu Araf Specialist Hospital, Lafia, Nigeria. akpanoah@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Akpa NE, Onwubiko VA, Tenmang PE, Odugbo PO, Wade PD. Client’s pre-operative expectations and outcome of cataract surgery at the Jos University Teaching Hospital, Jos, Plateau State, Nigeria. Glob J Cataract Surg Res Ophthalmol. doi: 10.25259/GJCSRO_36_2024
Abstract
Objectives:
A cataract is an opacity of the natural crystalline lens that causes vision loss. It is the most common cause of blindness worldwide, accounting for 39% of the 42 million blind people in the world. The optimum outcome from a cataract surgery can be achieved if post-operative subjective outcomes meet pre-operative expectations. It is expressed in different ways including patient satisfaction. This study evaluated clients’ pre-operative expectations and the outcome of cataract surgery at Jos University Teaching Hospital.
Materials and Methods:
A quasi-experimental, prospective hospital-based study that consecutively recruited 109 participants aged 18 years and above for 6 months. Data regarding the sociodemographic characteristics, pre-operative visual function, and expected post-operative outcome were collected preoperatively, and the subjective outcome and level of patient satisfaction were also assessed 6 weeks after surgery using a visual function index questionnaire. Data were analysed using the Statistical Package for the Social Sciences’ version 23. Frequencies and percentages were determined for categorical variables; mean and standard deviation, median, and interquartile range were calculated for continuous variables. Correlation was used to measure the relationship between overall satisfaction and expected or achieved visual function. A significant level was determined at P < 0.05.
Results:
A total of 109 participants were seen in this study, of which 60 (55%) were males. The mean age of participants in the study was 64.5 ± 11.1 years. The median (interquartile range) expected and actual post-operative outcome scores were 100 (80–100) and 98 (75–100), respectively. The majority of the participants, 86 (78.9%), were satisfied with the outcome of cataract surgery, and the predictors of satisfaction were insertion of posterior chamber intraocular lens, absence of complications, and absence of ocular comorbidities. We found a significant strong positive correlation between subjective outcome and satisfaction (r = 0.538, P ≤ 0.0001).
Conclusion:
The majority of the clients were satisfied with the outcome of their surgeries which meets the high expected outcomes from the clients pre-operative. Adequate counselling, training, and retraining of surgeons are key to improving and maintaining satisfaction with the outcome of cataract surgery.
Keywords
Pre-operative expectation
Cataract
Surgery
Outcomes
Client satisfaction
INTRODUCTION
Cataracts are the most common causes of blindness worldwide accounting for 39% (17 million) of the 42 million blindness in the world.[1] The definitive modality of treatment is surgery.[2] Cataract surgical rate (CSR) is the number of cataract surgeries performed per year per million population. As of 2015, CSR was about 317/year/million population in Nigeria.[3] This is far below the 2000–3000/year/million population recommended for Sub-Saharan Africa.[4]
Environmental and some individual factors and hurdles in the health system have contributed to the majority of people with cataracts not being able to access surgical intervention. The small proportion of those that have access to surgical intervention might not have the outcome they expected. Hence, the need for maximising the outcomes of cataract surgeries, as well as patient satisfaction, cannot be overemphasised. The optimum outcome from a cataract surgery can be achieved if post-operative subjective outcomes meet pre-operative expectations. It is expressed in different ways including patient satisfaction.[5]
Furthermore, as health care is fast becoming customer-oriented and competitive, patient’s satisfaction with the outcome of their cataract surgeries is very important. This is because they will recommend their healthcare providers to other clients, and positive feedback is important for the growth of any system.[6] Thus, improving the uptake of cataract surgery, thereby reducing the incidence of blindness from cataracts. There is a paucity of data on patients’ pre-operative expectations and the outcome of cataract surgery in Nigeria. We report on patients’ pre-operative expectations and the outcome of cataract surgery at Jos University Teaching Hospital (JUTH) to identify factors associated with patient satisfaction following cataract surgery.
MATERIALS AND METHODS
The study was a six (6) months prospective, quasi-experimental, hospital-based study. The sample size was calculated using the sample size estimation formula of two (2) independent means in the same sample (before and after an intervention).[7] The final sample size of 109 was obtained after adjusting for the expected response rate of 90%.
The study consecutively recruited adults (18 years and above) who were booked and showed up for cataract surgery during the study period of six (6) months. Participants with obviously complicated cataracts and those who were unable to define their expectations, outcomes, and satisfactions effectively were excluded.
Ethical approval was obtained from the Health Research Ethics Committee of JUTH. Written informed consent was also obtained from respondents before enrollment into the study.
A study identification number was assigned to all participants. Demographic data of the respondents, such as age, gender, place of residence, level of education, and occupation, were recorded.
The 14-item modified visual function index assessment (VF-14) questionnaire was used to assess the expected and actual outcome of the cataract surgery.[8] The responses allowed were ‘yes’ (when a patient has difficulty performing that activity) and ‘no’ (when a patient does not have difficulty performing that activity). For the activity that had a response of ‘no,’ the score given was 4. In the activity for which the response was ‘yes,’ the respondents were asked how much difficulty they currently had with the activity – ‘a little difficulty’ had a score of 3, ‘moderate difficulty’ had a score of 2, ‘great difficulty’ had a score of 1 and ‘unable to do it’ had a score of zero. An item was not included in the scoring system if the patient could not do that activity for reasons unrelated to their vision. Each scored item was then multiplied by 25 to a highest score of 100 (able to perform all applicable activities without any difficulty) and a lowest score of zero (unable to perform the applicable activity because of poor vision). This was how patients were asked to rate their pre-operative visual function on the day before surgery and the post-operative outcome at 6 weeks after surgery for each of the 14 items on the visual function index.
For the expected outcome, which was estimated on the day before surgery, patients who reported difficulty in performing an activity preoperatively were asked whether they thought there would be improvement after surgery. If the patient’s response was yes, he/she was asked to estimate how much improvement they expected. A little improvement had a score of 1, moderate improvement of 2, great improvement - a score of 3, and very great improvement had a score of 4. Each scored item was then multiplied by 25 to the highest score of 100 (able to perform all applicable activities without any difficulty) and the lowest score of zero (unable to perform the applicable activity because of poor vision) to give the expected postoperative outcome.
Grouping by median split method[9] was done where the expected post-operative or subjective post-operative visual outcome score was considered high if it was greater than or equal to the median score and low if it was less than the median score. If the subjective post-operative outcome score was at least as high as the expected outcome score, then the expectations were met. The surgeries were performed by the consultants and senior resident doctors (supervised by the consultants) in the unit using either small incision cataract surgery or conventional extracapsular cataract extraction and posterior chamber intraocular lens (IOL) implantation technique under sub-tenon’s local anaesthesia. However, in a few cases where the posterior capsular tear occurred, the anterior chamber IOL was implanted, or patients were left aphakic.
Satisfaction with the outcome
At six (6) weeks after surgery, patients were asked to rate their satisfaction with visual function for each item of the VF-14 index on a 5-point ordinal scale from 1 to 5 as follows: Very dissatisfied (1), Dissatisfied (2), Neither satisfied nor dissatisfied (3), Satisfied (4) and Very satisfied (5). The respondents who rated their satisfaction with the outcome of cataract surgery as 4 or 5 were considered satisfied, while those who recorded satisfaction with the outcome as 1 or 2 or 3 were regarded as dissatisfied.
Statistical analysis
All data collected were cleaned and analysed using the Statistical Package for the Social Sciences’ version 23. Frequencies and percentages were determined for categorical variables; mean and standard deviation, median, and interquartile range were calculated for continuous variables. Correlation was used to measure the relationship between overall satisfaction and expected or achieved visual function. A significant level was determined at P < 0.05.
Study definitions
Cataracts: Cataracts are opacities of the natural, crystalline lens that cause a reduction in vision.[10]
Expectations: Patients’ hopes or desires concerning clinical events.[11]
The outcome of cataract surgery: Consequence of surgical intervention for blindness from cataracts.[12]
Subjective outcome: What the patient does now that he/she could not do before the surgery.[12]
Patient satisfaction: How much benefit the patient feels from the surgery.[12]
Complicated cataracts: Cataracts that coexist with other ocular conditions that can affect the outcome of cataract surgery.[13]
RESULTS
A total of 109 participants were recruited for this study. The study comprised 60 (55.0%) male and 49 (45.0%) female participants. The overall mean ± standard deviation age was 64.5±11.1 years. Majority of the participants, 94 (86.2%) paid out-of-pocket [Table 1].
| Demographic variables | Frequency (%) |
|---|---|
| Age | |
| <50 | 6 (5.5) |
| 51–60 | 36 (33.0) |
| >60 | 67 (61.5) |
| Total | 109 (100.0) |
| Sex | |
| Male | 60 (55.0) |
| Female | 49 (45.0) |
| Total | 109 (100.0) |
| Occupation | |
| Retired civil servant | 33 (30.3) |
| Entrepreneurs | 30 (27.5) |
| Others | 16 (14.7) |
| Housewife | 13 (11.9) |
| Farmer | 10 (9.2) |
| Civil servant | 5 (4.6) |
| Student | 2 (1.8) |
| Total | 109 (100.0) |
| Address | |
| Urban | 85 (78.0) |
| Rural | 24 (22.0) |
| Total | 109 (100.0) |
| Literacy level | |
| Primary | 20 (18.3) |
| Secondary | 13 (11.9) |
| Tertiary | 40 (36.7) |
| None | 36 (33.0) |
| Total | 109 (100.0) |
| Payment method for surgery | |
| NHIS | 15 (13.8) |
| Out-of-pocket | 94 (86.2) |
| Total | 109 (100.0) |
| Religion | |
| Christianity | 78 (71.6) |
| Islam | 31 (28.4) |
| Total | 109 (100.0) |
NHIS: National Health Insurance Scheme
Slightly more than half, 55(50.5%) of the participants had high pre-operative visual function scores (a score of 71 and above) [Table 2].
| Variable | Frequency (%) | Median (IQR) |
|---|---|---|
| Pre-operative visual function | ||
| High | 55 (50.5) | 71 (57–93) |
| Low | 54 (49.5) | |
| Total | 109 (100.0) | |
| Expectation | ||
| High | 91 (83.5) | 100 (80–100) |
| Low | 18 (16.5) | |
| Total | 109 (100.0) | |
| Subjective outcome | ||
| High | 69 (63.3) | 98 (75–100) |
| Low | 40 (36.7) | |
| Total | 109 (100.0) |
Grouping by median split method (High ≥ Median; Low < Median); IQR = 25th–75th Percentiles. IQR: Interquartile range
The majority of the participants, 93(83.5%), had high pre-operative expectations, i.e., a score of 100 [Table 2].
Most of the participants, 69(63.3%), had high subjective outcomes of cataract surgery (a score of 98 and above) [Table 2].
The study showed that the majority of the participants (78.9%) were satisfied with the outcome of their surgery [Figure 1].
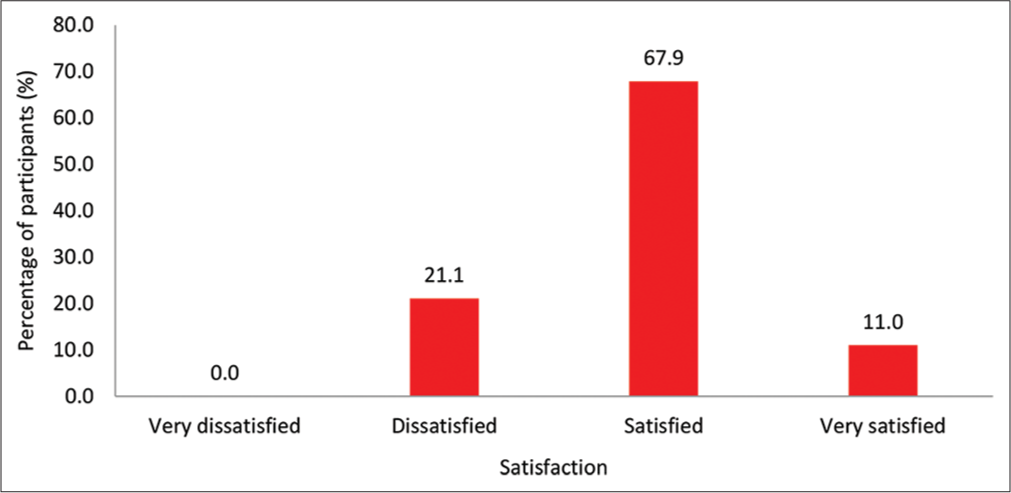
- Distribution of level of satisfaction.
There was no significant correlation between expectation and satisfaction (r = 0.140, P = 0.147) [Figure 2].
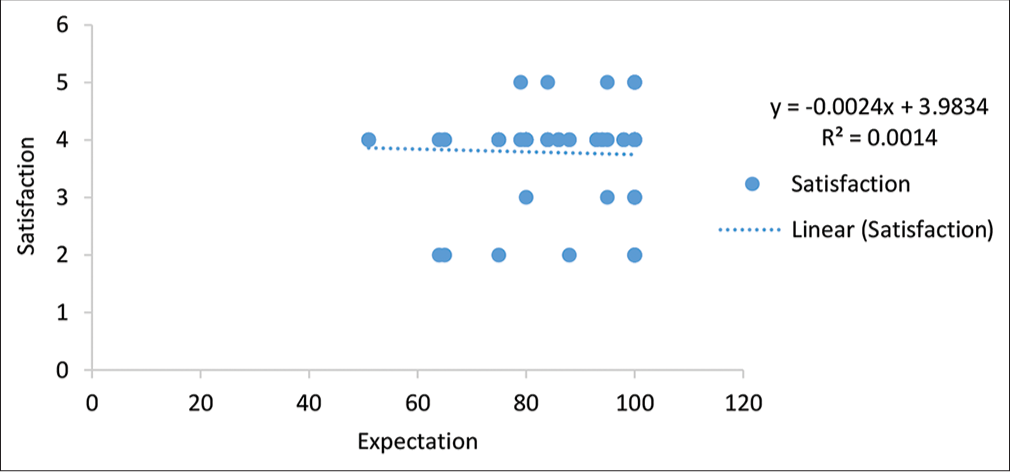
- Correlation between expectation and satisfaction.
The study revealed a positive, significant correlation between post-operative subjective outcome and patient satisfaction with the outcome of cataract surgery (r = 0.538, P ≤ 0.0001). [Figure 3].
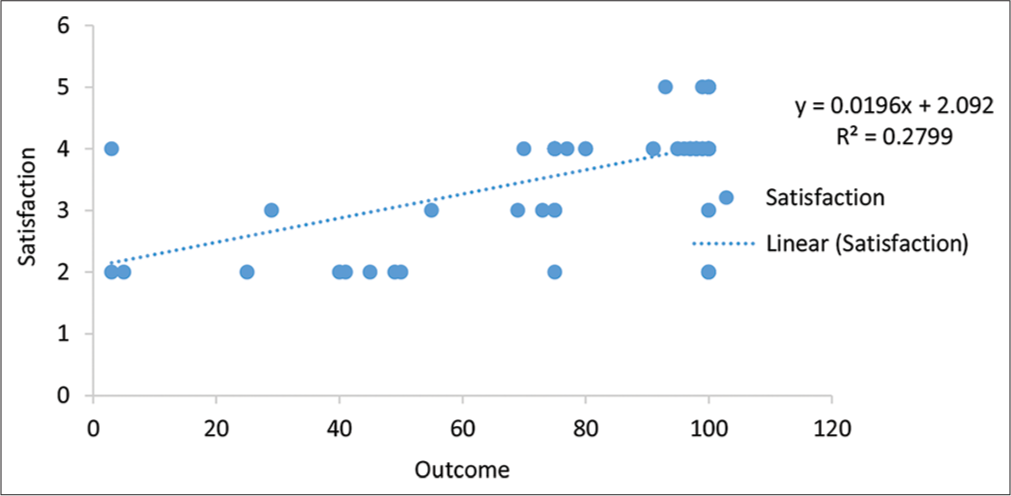
- Correlation between subjective post-operative outcome and satisfaction.
It was discovered that there was no statistically significant relationship between socio-demographic characteristics and level of satisfaction with the outcome of cataract surgery [Table 3].
| Predictors | Level of satisfaction | χ2 | Df | P-value | ||
|---|---|---|---|---|---|---|
| Satisfied | Dissatisfied | Total | ||||
| Age group (yrs.) | 3.437 | 2 | 0.179f | |||
| <50 | 3 (3.5) | 3 (13.0) | 6 (5.5) | |||
| 51–60 | 30 (34.9) | 6 (26.1)` | 36 (33.0) | |||
| >60 | 53 (61.6) | 14 (60.9) | 67 (61.5) | |||
| Sex | 0.614 | 1 | 0.433 | |||
| Male | 49 (57.0) | 11 (47.8) | 60 (55.0) | |||
| Female | 37 (43.0) | 12 (52.2) | 49 (45.0) | |||
| Religion | 0.079 | 1 | 0.778 | |||
| Christianity | 61 (70.9) | 17 (73.9) | 78 (71.6) | |||
| Islam | 25 (29.1) | 6 (26.1) | 31 (28.4) | |||
| Occupation | 4.959 | 6 | 0.532f | |||
| Farmer | 8 (9.3) | 2 (8.7) | 10 (9.2) | |||
| Retired civil servant | 28 (32.6) | 5 (21.7) | 33 (30.3) | |||
| Business/Artisan | 23 (26.7) | 7 (30.4) | 30 (27.5) | |||
| Student | 0 (0.0) | 2 (8.7) | 2 (1.8) | |||
| Housewife | 9 (10.5) | 4 (17.4) | 13 (11.9) | |||
| Civil servant | 5 (5.8) | 0 (0.0) | 5 (4.6) | |||
| Others | 13 (15.1) | 3 (13.0) | 16 (14.7) | |||
| Address | 0.141 | 1 | 0.707 | |||
| Urban | 68 (79.1) | 19 (82.6) | 87 (79.8) | |||
| Rural | 18 (20.9) | 4 (17.4) | 22 (20.2) | |||
| Literacy level | 4.855 | 3 | 0.183 | |||
| Primary | 13 (15.1) | 7 (30.4) | 20 (18.3) | |||
| Secondary | 9 (10.5) | 4 (17.4) | 13 (11.9) | |||
| Tertiary | 35 (40.7) | 5 (21.7) | 40 (36.7) | |||
| None | 29 (33.7) | 7 (30.4) | 36 (33.0) | |||
| Payment method for surgery | 0.013 | 1 | 0.910 | |||
| NHIS | 12 (14.0) | 3 (13.0) | 15 (13.6) | |||
| Out of pocket | 74 (86.0) | 20 (87.0) | 94 (86.2) | |||
NHIS: National Health Insurance Scheme, Df: Degree of freedom, f: Fisher’s exact, χ2: Chi-square
The univariate logistic regression showed the following factors to be significantly associated with satisfaction with the outcome of cataract surgery: posterior chamber IOL insertion, absence of ocular comorbidity, and complications [Table 4].
| Predictors | Level of satisfaction | χ2/f | Df | P-value | ||
|---|---|---|---|---|---|---|
| Satisfied | Dissatisfied | Total | ||||
| Surgeon | 0.770 | 1 | 0.380 | |||
| Ophthalmologist | 64 (81) | 15 (19) | 79 (100) | |||
| Resident/Trainee | 22 (73.3) | 8 (26.7) | 30 (100) | |||
| Total | 86 (78.9) | 23 (21.1) | 109 (100.0) | |||
| Type of surgery | 1 | 0.516f | ||||
| SICS | 75 (79.8) | 19 (20.2) | 94 (100) | |||
| ECCE | 11 (73.3) | 4 (26.7) | 15 (100) | |||
| Total | 86 (78.9) | 23 (21.1) | 109 (100.0) | |||
| IOL | 2 | 0.0001f | ||||
| PC-IOL | 83 (82.2) | 18 (17.8) | 101 (100) | |||
| AC-IOL | 3 (50) | 3 (50) | 6 (100) | |||
| No IOL | 0 (0.0) | 2 (100) | 2 (100) | |||
| Total | 86 (78.9) | 23 (21.1) | 109 (100.0) | |||
| Ocular morbidity | 4.359 | 1 | 0.037 | |||
| Present | 6 (54.5) | 5 (45.5) | 11 (100) | |||
| Absent | 80 (81.6) | 18 (18.4) | 98 (100) | |||
| Total | 86 (78.9) | 23 (21.1) | 109 (100.0) | |||
| Operative complications in operated eye | 17.994 | 1 | 0.001 | |||
| Present | 5 (35.7) | 9 (64.3) | 14 (100) | |||
| Absent | 81 (85.3) | 14 (14.7) | 95 (100) | |||
| Total | 86 (78.9) | 23 (21.1) | 109 (100.0) | |||
SICS: Small incision cataract surgery, ECCE: Extracapsular cataract extraction, IOL: Intraocular lens, AC-IOL: Anterior chamber intraocular lens, PC-IOL: Posterior chamber intraocular lens, f: Fisher’s exact, Df: Degree of freedom, χ2/f : Chi-square/Fisher’s exact.
Multiple logistic regression analysis revealed that IOL implantation (P = 0.019; odds ratio [OR] = 6.123, confidence interval [CI] = 1.352–27.737), absence of ocular comorbidities (P = 0.006; OR = 0.587; CI = 0.402–0.857) and absence of complications (P = 0.001; OR = 0.078; CI = 0.018–0.336) were independently associated with satisfaction [Table 5].
| Predictor variables | Satisfaction with outcome | |
|---|---|---|
| Adjusted odds ratio (95% CI) | P-value | |
| Surgeon | 0.965 (0.260–4.085) | 0.965 |
| Type of surgery | 2.575 (0.556–11.931) | 0.227 |
| Intraocular lens | 6.123 (1.352–27.737) | 0.019 |
| Comorbidity | 0.587 (0.402–0.857) | 0.006 |
| Complications | 0.078 (0.018–0.336) | 0.001 |
CI: Confidence interval
DISCUSSION
From this study, the mean age of the participants with cataracts is comparable with findings from similar studies in Nigeria[12] and India.[14] It agrees with the fact that older age is a risk factor for cataracts.[15]
The study had more male participants than females. This is similar to findings reported in previous studies in Plateau state-Nigeria[12] and India.[14] Possible explanations for this include males, usually being the head of the family, control the family resources and do not need to get permission before using or accessing health care.
Most participants paid out-of-pocket for the surgery. This underscores the low coverage of the National Health Insurance Scheme in Nigeria.
The majority of the participants had high expectations of the post-operative outcome of the cataract surgery. This was corroborated in previous studies in Ethiopia,[6] United Kingdom,[9] China,[16] USA[17] and Australia.[5]
The following factors could be responsible for the high expectations participants expressed: Jos University Teaching Hospital is a tertiary hospital considered by many to have highly skilled doctors and high-tech equipment, so participants might see no reason why they should not expect the best outcome. The participants could obtain information from persons who had their cataract surgery in JUTH with a good outcome. Moreover, since the majority paid out-of-pocket, they would expect value for their money. All these factors could have informed their decision to have high expectations.
Hence, comprehensive counselling is necessary for all patients undergoing cataract surgery. “Under-promise and over-deliver” are good strategies for managing patients’ expectations.
The majority of the participants in this study had high subjective post-operative outcomes. This could be because of the high level of competence of the surgeons. On the other hand, the exclusion of complicated cataracts, which can poorly prognosticate the outcome, could also be responsible. In like manner, previous studies in Nigeria,[8,11] Ethiopia[6], and Australia[5] reported great improvement in visual function after cataract surgery.
Most participants were satisfied with the outcome of the cataract surgery. It could be due to the fulfilment of their expectations regarding the outcome of cataract surgery.
This is consistent with what was reported in Nigeria,[11] and Japan.[18]
This study found the following factors to be predictors of satisfaction with the outcome of cataract surgery – implantation of IOL, absence of complications, and absence of ocular comorbidities. These factors, including subjective outcome, are major sources of patient satisfaction with the outcome of cataract surgery. Previous studies in Ethiopia[6], the USA[17], and China[16] found ocular comorbidity to be predictors of patient satisfaction.
The limitation of the study was that the sample size was small and the short duration of the study.
Recommendation
The following recommendations were made to increase awareness of ophthalmologists in addressing patient expectations regarding the outcome of cataract surgical services. Training and retraining of surgeons are to improve surgical skills and reduce complications. These will enhance patient satisfaction and improve cataract surgical uptake.
CONCLUSION
The majority of the participants were satisfied with the outcome of the cataract surgery despite their high expectations. The predictors of patient satisfaction with the outcome of cataract surgery included implantation of IOL, absence of complications, and absence of ocular comorbidities.
Ethical approval
The research/study approved by the Institutional Review Board at Jos University Teaching Hospital, number JUTH/DCS/IREC/127/XXXI/2181, dated 6th April 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Vision 2020-the right to sight: How much has been achieved in Nigeria? And what next? Niger J Med. 2022;31:366-70.
- [CrossRef] [Google Scholar]
- Increasing sustainable cataract services in sub-Saharan Africa: an experimental initiative. Community Eye Health. 2014;27:73.
- [Google Scholar]
- Randomised controlled trial of preoperative information to improve satisfaction with cataract surgery. Br J Ophthalmol. 2005;89:10-3.
- [CrossRef] [PubMed] [Google Scholar]
- Patients' preoperative expectation and outcome of cataract surgery at Jimma University Specialised hospital-department of Ophthalmology. Ethiop J Health Sci. 2011;21:47-56.
- [CrossRef] [PubMed] [Google Scholar]
- Sample size determination In: Research methodology and dissertation writing for health and allied health professionals. Abuja, Nigeria: Cress Global Link Limited; 2009. p. :70-5.
- [Google Scholar]
- Quality-of-life and visual function after manual small incision cataract surgery in South Western Nigeria. West Afr J Med. 2012;31:114-9.
- [Google Scholar]
- Refractive expectations of patients having cataract surgery. J Cataract Refract Surg. 2005;31:1970-5.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life of cataract patients before and after surgery-evidence from four rural communities in Ghana. Mathews J Ophthalmol. 2016;1:1-7.
- [Google Scholar]
- Patients' expectations for medical care: An expanded formulation based on a review of the literature. Med Care Res Rev. 1996;53:3-27.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of cataract surgery on quality of life in Plateau State, Nigeria. Niger J Ophthalmol. 2009;17:5-10.
- [CrossRef] [Google Scholar]
- Visual outcome of cataract surgery from a free outreach camp among rural areas of Southern-Kaduna Nigeria. Glob J Cataract Surg Res Ophthalmol. 2022;1:15-20.
- [CrossRef] [Google Scholar]
- Cataract surgery visual outcomes and associated risk factors in secondary level eye care centers of LV Prasad Eye Institute, India. PLoS One. 2016;11:1-11.
- [CrossRef] [PubMed] [Google Scholar]
- Outcome of manual small incision cataract surgery in a hospital in southern Nigeria. South Afr Ophthalmol J. 2019;14:17-9.
- [Google Scholar]
- Preoperative expectations and postoperative outcomes of visual functioning among cataract patients in urban southern China. PLoS One. 2017;12:1-14.
- [CrossRef] [PubMed] [Google Scholar]
- Preoperative functional expectations and postoperative outcomes among patients undergoing first eye cataract surgery. Arch Ophthalmol. 1995;113:1312-8.
- [CrossRef] [PubMed] [Google Scholar]
- Changes in patient subjective happiness and satisfaction with cataract surgery. Sci Rep. 2020;10:1-8.
- [CrossRef] [PubMed] [Google Scholar]






