Translate this page into:
Intraocular lens opacification: An uncommon case scenario
*Corresponding author: Deepak Mishra, Regional Institute of Ophthalmology, Institute of Medical Sciences, Banaras Hindu University, Varanasi, Uttar Pradesh, India. drdmishra12@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Tiwari K, Pal K, Mishra D, Reddy MY. Intraocular lens opacification: An uncommon case scenario. Glob J Cataract Surg Res Ophthalmol. doi: 10.25259/GJCSRO_40_2024
Abstract
Intraocular lens (IOL) opacification is a rare complication of cataract surgery. It can cause significant deterioration of visual performance. We report a case of a 50-year-old female with right eye (RE) primary IOL opacification, who presented to us 6 months after cataract surgery with whole IOL opacification. The patient was managed by RE IOL exchange. The purpose of this case report is to spread awareness about this complication related to cataract surgery and provide insight into its management.
Keywords
Lens opacification
Intraocular lens exchange
Cataract
INTRODUCTION
Intraocular lens (IOL) opacification is a relatively rare and a new complication of cataract surgery. It is described as an alteration in lens transparency due to opacification of the IOL surface or IOL material, which further leads to deterioration of the patient’s visual acuity.[1] It is important to have a detailed evaluation and identification of such cases as it can lead to misdiagnosis, resulting in undue interventional procedures.[2] Different types of opacifications have been reported in the past few years. It can be due to crystalline deposits during cataract surgery, coating of lenses with silicone oil in cases of vitreoretinal surgeries, or due to ophthalmic ointment penetration into the anterior chamber postoperatively.[3,4] Few cases of dystrophic calcification of the lens with the formation of calcified deposits on the posterior surface of the lens have been documented but were mostly associated with asteroid hyalosis.[5,6] Opacification can involve just the optic, haptic or lens in toto. Different patterns have been observed in various types of IOL biomaterials, such as snowflake opacification in polymethyl methacrylate IOLs, discolouration in Silicone IOLs, calcification in hydrophilic acrylic IOLs and glistenings in hydrophobic acrylic IOLs.[7,8] It can present intraoperatively, early or late postoperatively. Each of them has different aetiologies depending on the time of presentation. Intraoperative finding is mainly related to viscoelastic substances or balanced salt solutions.[9] Early post-operative presentation could be due to the interaction of hydrogel materials with dyes. Glistenings and calcification are late presentations which are fluid-filled microvacuoles seen in hydrophobic IOLs and precipitated calcium and phosphate on or within IOL, respectively.[10] Risk factors associated could be local, such as chronic uveitis, glaucoma, keratoplasty procedures or systemic associations such as diabetes and hypertension or IOL-related factors such as biomedical impurities.[10-15]
CASE REPORT
A 50-year-old female presented to us with complaints of diminution of vision in both eyes (right eye [RE] more than the left eye [LE]) for 8 years and whitish opacity in the RE for 3 years. There is a history of RE and LE cataract surgery 10 years and 4 years ago, respectively. There is a history of joint pain for which the patient was consulting an orthopaedist and was being treated for osteoarthritis. There is no history of any other systemic illness. There is a family history of similar complaints in one of her relatives who was operated on for cataracts in the same hospital. There is no significant drug intake history.
On torch light examination, a white pupillary reflex was seen in RE appearing to be a hypermature cataract. Further examination was done after dilating both eyes. On slit-lamp examination, totally opacified IOL was seen in RE and clear IOL was seen in LE [Figure 1].
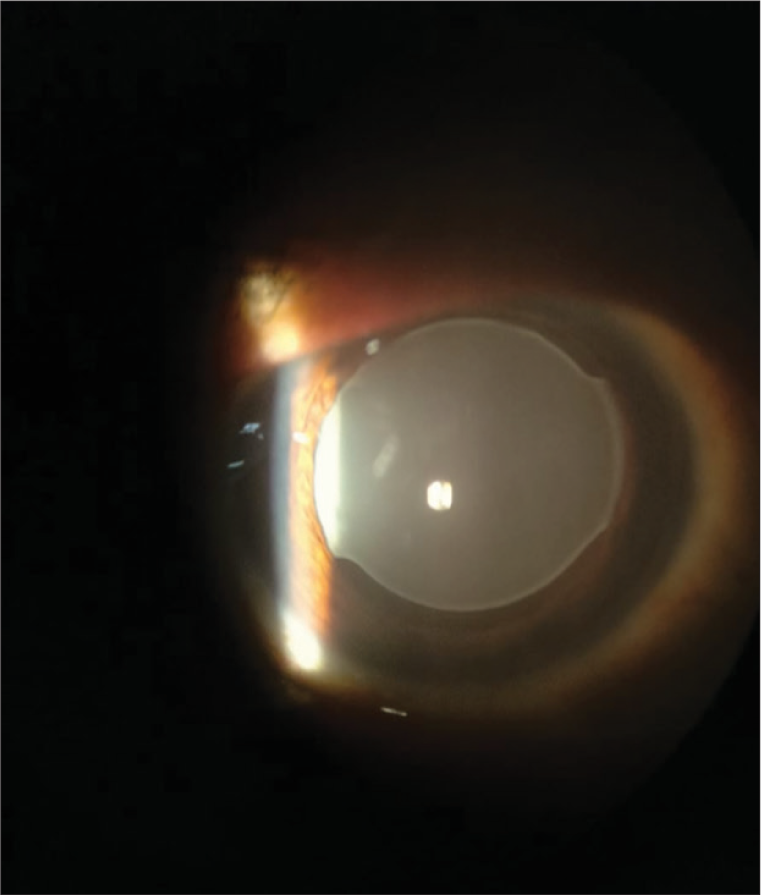
- Opacified intraocular lens on slit-lamp examination.
Routine blood investigation: Viral markers (human immunodeficiency virus, hepatitis B surface antigen and anti-hepatitis C virus) – Non-reactive
Random blood sugar: 110 mg/dL
Complete blood count: Within normal limit
Erythrocyte sedimentation rate: 15 mm/h
C-reactive protein: 0.5 mg/dL
Best-corrected visual acuity: RE – Hand movement close to face,
Perception of light (PL) – Present
Projection of rays (PR) – Accurate
Best-corrected visual acuity: LE – 6/12 partial
Perception of light (PL) – Present
Projection of rays (PR) – Accurate
Pupil: Both eye (BE) – Normal shape/Normal reaction
Intraocular Pressure (IOP): RE – 12 mmHg
LE – 12 mmHg
Anterior Chamber (AC): BE – Quiet
Fundus: RE – Details not clear due to media opacity
LE – No abnormality detected
On the basis of these findings, the patient was planned for RE IOL exchange surgery.
Intraoperatively, a 6–7 mm size tunnel was made superiorly and IOL was extracted as seen in Figures 2a and b. Opacified IOL was extracted in toto and sent for histopathological examination, as seen in Figure 2c. The posterior capsule was found to be intact after explantation. Therefore a hydrophobic lens was implanted in the capsular bag as seen in Figure 3. The patient was given topical steroids, non-steroidal anti-inflammatory drugs, and intraocular pressure-lowering drugs for post-operative inflammation.
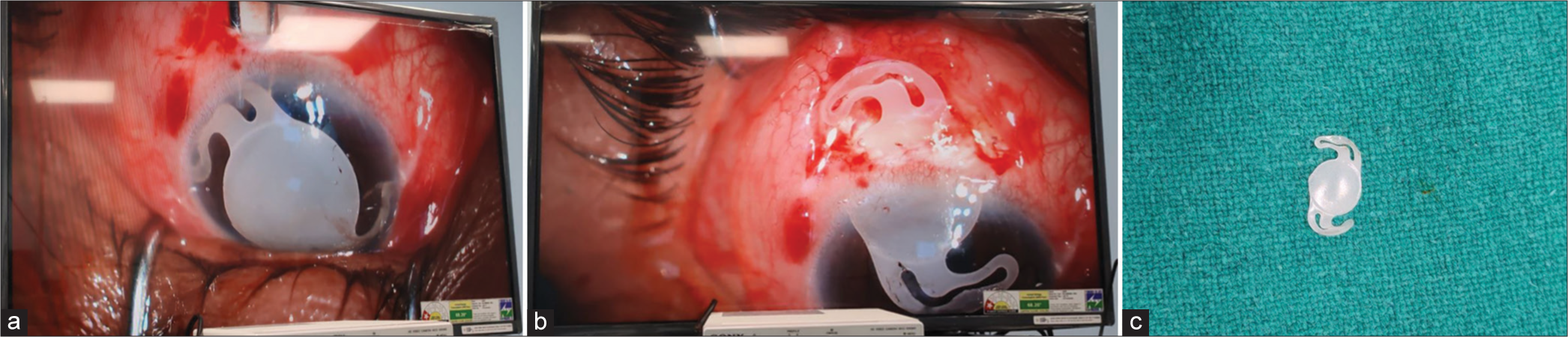
- (a) Opacified intraocular lens (IOL) in the anterior chamber. (b) Opacified IOL was extracted through the 6–7 mm scleral tunnel. (c) Opacified IOL extracted in toto.
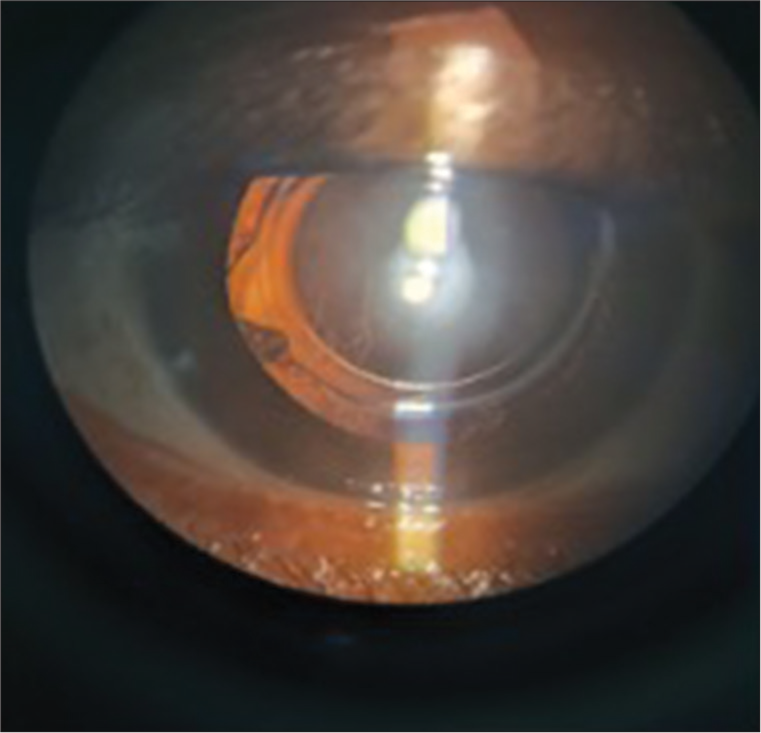
- Hydrophobic intraocular lens implantation in the capsular bag.
IOL was sent for laboratory diagnosis, which revealed calcium deposits.
DISCUSSION
The importance of IOL performance and lifelong transparency has progressively increased with the advent of early cataract surgery in the paediatric as well as in the adult population. Ideal IOL material should be biocompatible and stable to the host’s reaction to it. Therefore, constant research and development are required in the biomaterial of lenses to provide prolonged, better refractive outcomes.
IOL opacification, even though rare, is a recognised complication following cataract surgery. In our case, the opacification was attributed to calcific deposits on the IOL haptic and optic surfaces. Many speculations have been made regarding the exact mechanism of IOL opacification. It is found to be multifactorial. Many ophthalmologists have been reporting similar cases of opacification with various theories as the predisposing cause of opacification. The duration between surgery and the onset of IOL opacification ranged from 1 month to 6 years.[16]
Neuhann et al. described three varieties of IOL opacification. The first is primary, which is due to the fabrication of the IOL in its packaging process or inadequate formulation of the polymer. The secondary form is due to environmental circumstances, vitreoretinal surgeries, and systemic diseases, which can cause fluid-gas exchange and disrupt the blood-aqueous barrier. The third variety is false-positive calcification, when another pathology is mistaken for calcification or false-positive staining for calcium takes place.[17]
In a study by Bhattacharjee et al., using scanning electron microscopic and energy-dispersive spectroscopic findings, hydrophobic acrylic IOLs were evaluated. They concluded that hydrolytic biodegradation of these lens polymers in ocular media was responsible for delayed post-operative opacification and visual loss.[18]
Similar cases were reported by Tanaka et al., who described the opacification of silicone lenses in detail.[19] Mamalis published a report on calcified hydrophilic acrylic IOLs, which suggested the disintegration of ultraviolet (UV)-filter chromoform in IOL as the contributory cause.[20] Dorey et al. demonstrated a connection between calcium deposits and silicone which acted as a nidus within IOLs.[21] A report by Scherer et al. quoted that hydrophilic acrylate IOLs were prone to calcification as well. The high hydration of hydrophilic acrylate IOLs causes ionisation of their hydrophilic groups, leading to calcium ion complex formation on and within the material.[22] Kanclerz et al. found that age at the time of implantation also contributed to IOL calcification.[23] The opacified regions of IOL were found to be soaked in the aqueous humour, which led to the belief in its importance in the pathogenesis of opacification. Factors such as patient age, diabetes, prolonged post-operative duration, and inadequate packaging and storage of IOL were found to be contributing to the pathology. Dhaliwal et al. reported glistenings in AcrySof hydrophobic acrylic IOLs for the 1st time.[24] Wang et al. credited changes in the temperature of the surrounding environment as the cause for the vacuolation of IOL.[25] Gurabardhi et al. described calcification in a few designs of IOL by Oculentis and concluded that manufacturing issues could be the reason behind opacification.[26]
In a study by Mattová et al. on opacified MemoryLens IOLs, they found the absence of UV absorber and increased concentrations of low-molecular-weight components generated during the degradation of the polymer in a spectrophotometer analysis of such IOLs. Deficiency of protection against UV radiation led to subsequent polymer disintegration which was the proposed cause of the opacification.[1]
A few cases of acute IOL clouding were also reported in a study by Wang et al. They were all hydrophilic acrylate lenses with a hydrophobic surface. The copolymer materials of the IOL seemed to be susceptible to temperature changes which might have led to the temporary clouding of lenses.[25]
A study by Xie et al. found that calcium and phosphorus deposition was one of the main causes of hydrophilic acrylic IOL opacification. They performed IOL replacement surgery, which was very efficacious in improving the visual acuity of such patients.[27]
Since we have reported just a single case of IOL opacification, we could not analyse the IOL characteristic in much detail and provide a statistical report in relation to IOL material with opacification in our case. Since our patient had no history of any ocular surgery or report of any other ocular pathology in the duration after cataract surgery, it was probably the primary calcification of IOL.
CONCLUSION
IOL opacification, although rare, can significantly impair visual performance following cataract surgery. Our case highlights the occurrence of primary IOL opacification in a 50-year-old female attributed to calcific deposits on the IOL surfaces. The opacification led to substantial visual deterioration and necessitated an IOL exchange to restore vision. This case underscores the importance of recognising and managing IOL opacification as a potential complication. Continued research into IOL biomaterials and their interactions with ocular environments is essential to prevent and address such issues effectively.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
Dr. Deepak Mishra is on the editorial board of the Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Opacification of hydrophilic MemoryLens U940A intraocular lenses: Analysis of 2 explanted lenses. J Cataract Refract Surg. 2004;30:1934-9.
- [CrossRef] [PubMed] [Google Scholar]
- Causes of intraocular lens opacification or discoloration. J Cataract Refract Surg. 2007;33:713-26.
- [CrossRef] [PubMed] [Google Scholar]
- Toxic anterior segment syndrome and possible association with ointment in the anterior chamber fol lowing cataract surgery. J Cataract Refract Surg. 2006;32:227-35.
- [CrossRef] [PubMed] [Google Scholar]
- Late opacification of a silicone intraocular lens caused by ophthalmic ointment. J Cataract Refract Surg. 2006;32:341-6.
- [CrossRef] [PubMed] [Google Scholar]
- Surface calcification of silicone plate intraocular lenses in patients with asteroid hyalosis. Am J Ophthalmol. 2004;137:979-87.
- [CrossRef] [PubMed] [Google Scholar]
- Opacification of a silicone intraocular lens caused by calcium deposits on the optic. J Cataract Refract Surg. 2004;30:517-20.
- [CrossRef] [PubMed] [Google Scholar]
- Population based analysis of intraocular lens exchange and repositioning. J Cataract Refract Surg. 2017;43:754-60.
- [CrossRef] [PubMed] [Google Scholar]
- Glistenings and surface light scattering in intraocular lenses. J Cataract Refract Surg. 2010;36:1398-420.
- [CrossRef] [PubMed] [Google Scholar]
- Crystallization on intraocular lens surfaces associated with the use of Healon GV. Arch Ophthalmol. 1994;112:1037-42.
- [CrossRef] [PubMed] [Google Scholar]
- Postoperative intraocular lens opacification. Taiwan J Ophthalmol. 2018;8:49-51.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular lens calcification: Clinico-pathological report of two cases and literature review. J Ophthalmic Vis Res. 2018;13:195-9.
- [CrossRef] [PubMed] [Google Scholar]
- A narrative review of intraocular lens opacifications: Update 2020. Ann Transl Med. 2020;8:1547.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular lens exchange through a 3.2-mm corneal incision for opacified intraocular lenses. Indian J Ophthalmol. 2011;59:17-21.
- [CrossRef] [PubMed] [Google Scholar]
- Total opacification of intraocular lens implant after uncomplicated cataract surgery: A case series. Arch Ophthalmol. 2004;122:782-4.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of cataract and refractive surgery: A clinicopathological documentation. Trans Am Ophthalmol Soc. 2001;99:95-107.
- [Google Scholar]
- Calcification of a hydrophilic acrylic intraocular lens after Descemet-stripping endothelial keratoplasty: Case report and laboratory analyses. J Cataract Refract Surg. 2013;39:799-803.
- [CrossRef] [PubMed] [Google Scholar]
- A new classification of calcification of intraocular lenses. Ophthalmology. 2008;115:73-9.
- [CrossRef] [PubMed] [Google Scholar]
- Delayed postoperative opacification of three hydrophobic acrylic intraocular lens: A scanning electron microscopic and energy dispersive spectroscopic study. Indian J Ophthalmol. 2021;69:1103-7.
- [CrossRef] [PubMed] [Google Scholar]
- Brown haze in an Allergan SI-40NB silicone intraocular lens. J Cataract Refract Surg. 2004;30:250-2.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of foldable intraocular lenses requiring explantation or secondary intervention--2001 survey update. J Cataract Refract Surg. 2002;28:2193-201.
- [CrossRef] [PubMed] [Google Scholar]
- Proposed pathogenesis for the delayed postoperative opacification of the hydroview hydrogel intraocular lens. Am J Ophthalmol. 2003;135:591-8.
- [CrossRef] [PubMed] [Google Scholar]
- Serial opacification of a hydrophilic-hydrophobic acrylic intraocular lens: Analysis of potential risk factors. J Cataract Refract Surg. 2020;46:1624-9.
- [CrossRef] [PubMed] [Google Scholar]
- A review of late intraocular lens opacifications. Curr Opin Ophthalmol. 2021;32:31-44.
- [CrossRef] [PubMed] [Google Scholar]
- Visual significance of glistenings seen in the AcrySof intraocular lens. J Cataract Refract Surg. 1996;22:452-7.
- [CrossRef] [PubMed] [Google Scholar]
- Intraoperative and postoperative intraocular lens opacifications: Analysis of 42545 cases. J Ophthalmol. 2021;2021:1285947.
- [CrossRef] [PubMed] [Google Scholar]
- Serial intraocular lens opacifications of different designs from the same manufacturer: Clinical and light microscopic results of 71 explant cases. J Cataract Refract Surg. 2018;44:1326-32.
- [CrossRef] [PubMed] [Google Scholar]
- Late postoperative opacification of a new type hydrophilic acrylic intraocular lens. Adv Ophthalmol Pract Res. 2023;3:134-40.
- [CrossRef] [PubMed] [Google Scholar]







