Translate this page into:
A study of spectacle compliance in school going children of rural areas of south Gujarat
*Corresponding author: Uma Kavin Shroff, Department of Ophthalmology, Tejas Eye Hospital, Surat, Gujarat, India. umagajiwala@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Shroff UK, Gajiwala UR, Shroff KN, Prajapati VK, Choudhary T, Patel P. A study of spectacle compliance in school going children of rural areas of south Gujarat. Glob J Cataract Surg Res Ophthalmol. 2025;4:11-6. doi: 10.25259/GJCSRO_31_2024
Abstract
Objectives:
The primary objective of the study was to assess the compliance of spectacle wear among school children in rural areas of south Gujarat. Secondary objectives included identifying various factors affecting compliance and comparing compliance between children with different levels of visual acuity.
Materials and Methods:
This cross-sectional observational study was conducted in schools in rural south Gujarat. The study included students from 5th to 9th standard who had been prescribed glasses within the past 6 months to 1 year through a school eye screening program. A total of 333 children were recruited, and data were collected using a pre-designed, pre-tested and semi-structured questionnaire over 2 months (November to December 2018). Compliance was defined as wearing spectacles for the entire school day on at least 5 days a week. Observations were made regarding whether the student was wearing spectacles at the time of the survey, and visual acuity was measured using an illuminated Snellen chart. The power of prescribed spectacles was noted using a lensometer. Statistical analysis was performed using the Statistical Package for the Social Sciences software version 17.0, with P < 0.05 considered statistically significant.
Results:
Out of the 333 students, the compliance rate for spectacle wear was found to be 50.20%. Of the students, 148 were boys and 185 were girls, with a mean age of 12.42 years (standard deviation ±1.265). Observations indicated that 50.20% were wearing glasses at the time of the survey, 12.9% had forgotten them at home and 34.2% did not have spectacles. Compliance was higher among children with visual acuity worse than 6/12 (53.90%) compared to those with better visual acuity (34.37%). Children with binocular visual acuity worse than 6/12 showed a compliance rate of 61.30%, compared to 32.85% for those with monocular visual acuity worse than 6/12. There was no significant difference in compliance based on gender. Compliance varied by grade level, but no significant association could be established, with the highest compliance observed in the 9th grade (71.42%) and the lowest in the 6th grade (39.06%). Distance from the spectacle dispensing centre did not significantly affect compliance.
Conclusion:
Compliance with spectacle wear among school children in rural south Gujarat is suboptimal, with only 50.2% of students adhering to their prescribed use. Key factors influencing compliance include visual acuity, age and possibly the aesthetic appeal of the spectacles. Interventions to improve compliance should include enhanced screening programs, greater parental involvement and education, improved accessibility to spectacles, cost-sharing strategies and efforts to reduce the social stigma associated with wearing glasses. By addressing these multifaceted issues, it is possible to significantly improve compliance rates, ensuring better visual health and academic performance among children; this, in turn, represents a valuable investment in the future well-being and productivity of the population.
Keywords
Community ophthalmology
Refractive error
School screening
Spectacle compliance
INTRODUCTION
Uncorrected refractive error (URE) is the leading cause of vision impairment and the second leading cause of blindness globally,[1] affecting 1 in 90 people of all ages.[2] Available evidence indicates that URE in school-aged children continues to be a major public health problem in India.[2,3] School screening for refractive errors is one of the most important initiatives outlined in the World Health Organization (WHO) Vision 2020[4] targets for control of avoidable visual impairment in children. Correction of refractive error brings forth many desirable outcomes in children, such as better academic performance, better participation in activities, overall personality development and self-confidence, and becoming a better individual as a youth. Hence, addressing refractive errors in children is, in fact, an ‘investment in the country’s better future.’ The government has included refractive error check-ups under the school health program and the provision of free-of-cost spectacles to all children who are found to have refractive errors. Whether free spectacle distribution is the solution to this problem? The non-compliance rate is found to be as high as 65–70% in different studies carried out across the country.[5-7] Most of the time, energy and effort spent on school screening activities go to waste. The primary objective of the study was to assess the compliance of spectacle wear among school children. The secondary objectives were to study the various factors affecting compliance and to compare compliance between children with visual acuity <6/12 versus >6/12.
MATERIALS AND METHODS
It was a cross-sectional observational study carried out in schools in rural areas of south Gujarat. A due approval was taken from the concerned ethics committee. The students recruited for the study belonged to standard 5–9th and had been prescribed glasses within 6 months to 1 year through the school eye screening program. Inclusion and exclusion criteria, as mentioned below, had been followed. The data of 333 children were collected using a pre-designed, pre-tested and semi-structured questionnaire within the study period of 2 months, that is, November and December 2018.
The definition of compliance was taken as wearing spectacles for entire school hours on ≥5 days a week. At first, an observation was made whether the student was wearing spectacles or not at the time of filling out the questionnaire. If not, whether they had brought spectacles to school, had them at home, or did not have spectacles. Unaided visual acuity, as well as visual acuity with glasses, were noted on illuminated Snellen’s chart from a distance of 6 m by two ophthalmic assistants. The power of the spectacles prescribed was noted using a lensometer.
Inclusion criteria
The following criteria were included in the study:
Students of schools in rural areas of south Gujarat who have been screened and prescribed spectacles under the school screening program
Students of 5–9th standard
Those who have been prescribed glasses within 6 months to 1 year through a school eye screening program.
Exclusion criteria
The following criteria were excluded from the study:
Mentally challenged children
Those who have bought spectacles from outside on their own
Those who were absent from school on that particular day
Those who are prescribed spectacles in less than 6 months
Those who have been screened but not yet provided with spectacles
Half-filled forms.
A total of 333 children were included in the study and the data was collected using a pre-designed, pre-tested and semi-structured questionnaire.
The questionnaire had questions regarding basic demographic data, the source of spectacle procurement and its distance from the child’s residence. It also had questions regarding the duration of spectacle use as well as whether they were using it regularly or not. Barriers as well as facilitating factors to spectacle wear were asked. The data were compiled in the Microsoft Excel sheet and statistical analysis was performed by SPSS software version 17.0. Descriptive analysis was represented in the form of mean ± standard deviation (SD) for normally distributed variables. Normally distributed variables were compared by t-test, non-parametric variables by Mann–Whitney U test and categorical variables by Chi-square test. P < 0.05 was considered statistically significant for this study.
RESULTS
Out of the 333 students, the compliance rate for spectacle wear was found to be 50.20%. Of the students, 148 were boys and 185 were girls. The age-wise distribution of students was as follows [Figure 1], with a mean age of 12.42 years (SD ± 1.265). Observations indicated that 50.20% were wearing glasses at the time of the survey, 12.9% had forgotten them at home and 34.2% did not have spectacles [Figure 2]. The total compliance among school-going children was calculated to be 50.2% [Figure 3]. No significant statistical correlation was noted between gender and compliance with glasses [Figure 4]. Compliance was higher among children with visual acuity worse than 6/12 (53.90%) compared to those with better visual acuity (34.37%) [Figure 5a and Table 1a].
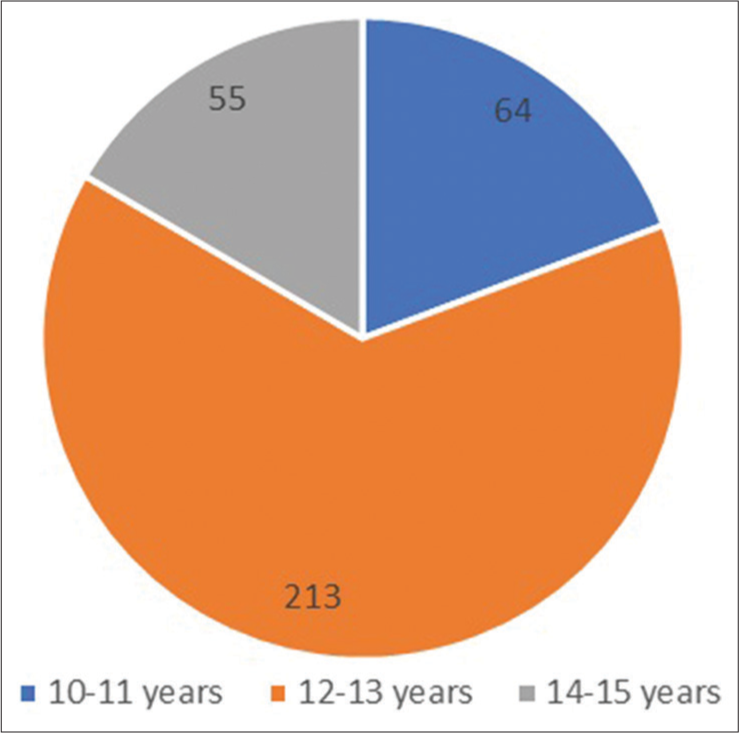
- Age-wise distribution of students.
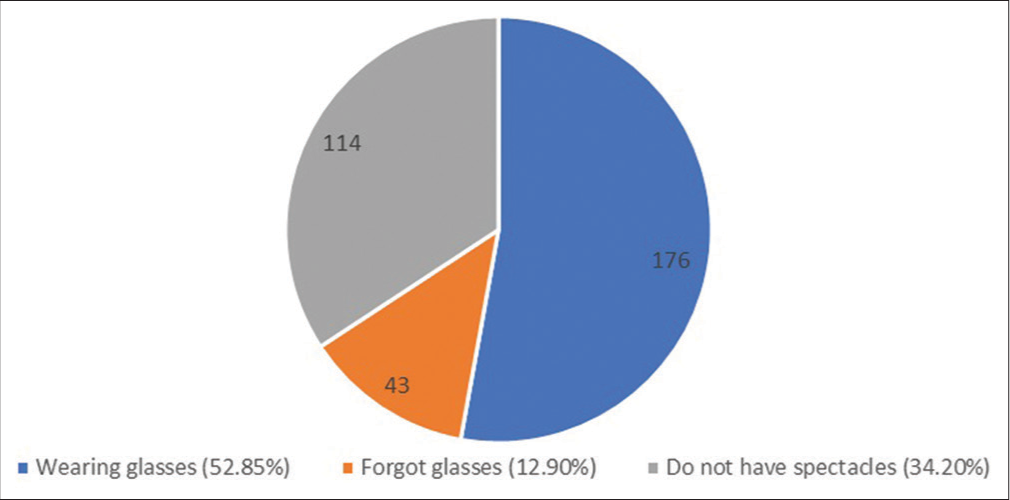
- Observations made regarding the compliance.
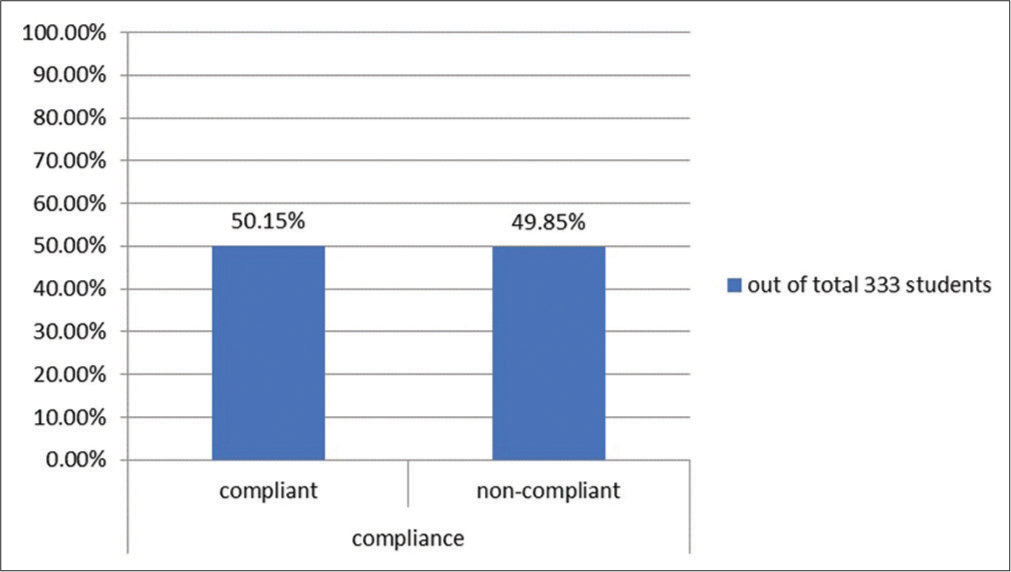
- Total compliance out of 333 students.
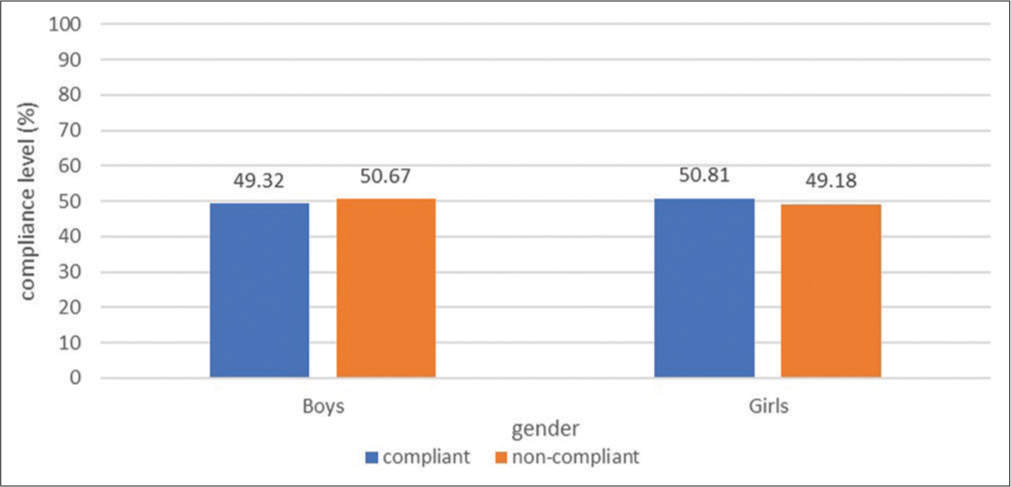
- Gender-wise compliance.
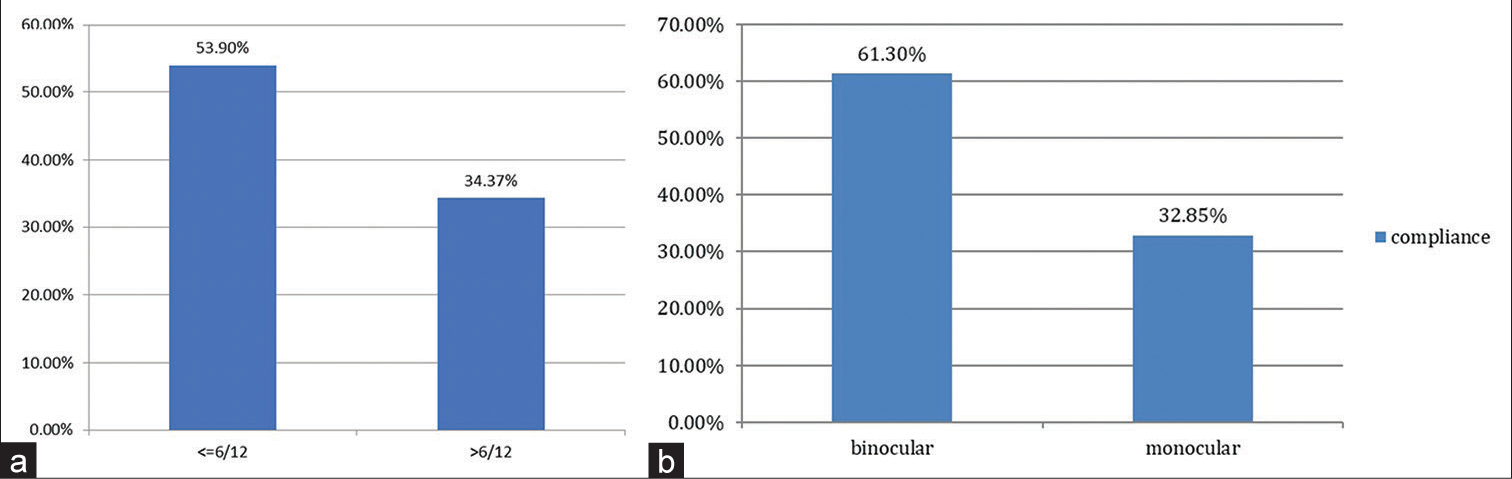
- Comparison of (a) compliance in children with visual acuity (VA) ≤6/12 versus >6/12. (b) Compliance in children with VA monocular versus binocular <6/12.
| VA | % Compliance |
|---|---|
| ≤6/12 | 53.90% (145 out of 269 children) |
| >6/12 | 34.37% (22 out of 64 children) |
VA: Visual acuity
Children with binocular visual acuity worse than 6/12 showed a compliance rate of 61.30%, compared to 32.85% for those with monocular visual acuity worse than 6/12 [Figure 5b and Table 1b]. Compliance varied by grade level, but no significant association could be established, with the highest compliance observed in the 9th grade (71.42%) and the lowest in the 6th grade (39.06%) [Figure 6]. Distance from the spectacle dispensing centre did not significantly affect compliance [Figure 7]. The barriers to spectacle compliance were lack of motivation, lack of counselling, cosmetic stigma, usefulness not established, broken/lost glasses, peer pressure, etc. Out of all non-compliant children, 54% reported broken glasses, 23% had broken frames, 11% were being teased by friends, 5% reported lost spectacles and 4% disliked the spectacle frame [Figure 8].

- Compliance rates across different grades.
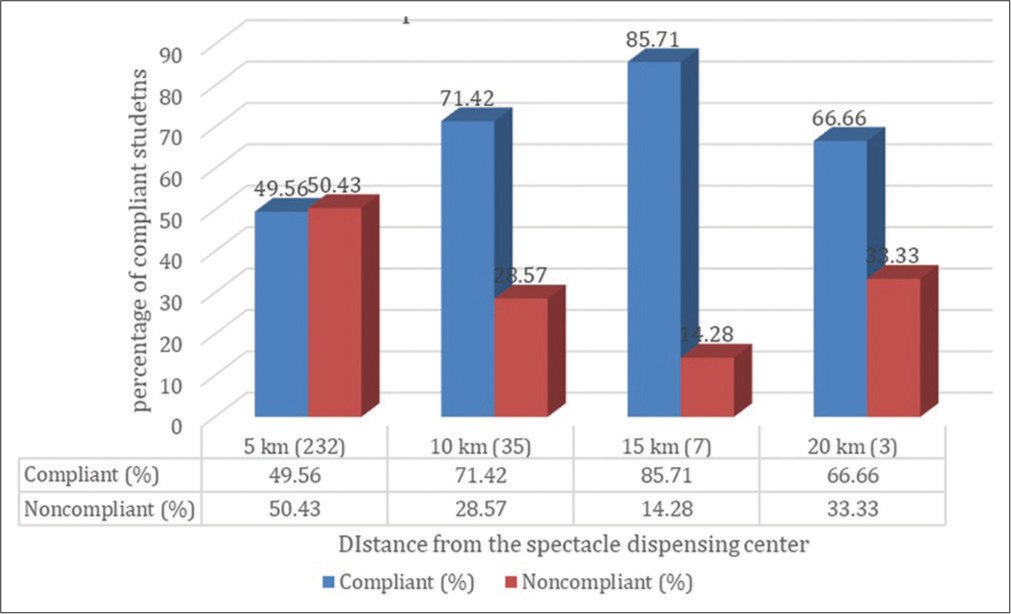
- Compliance rates based on distance from the spectacle centre.
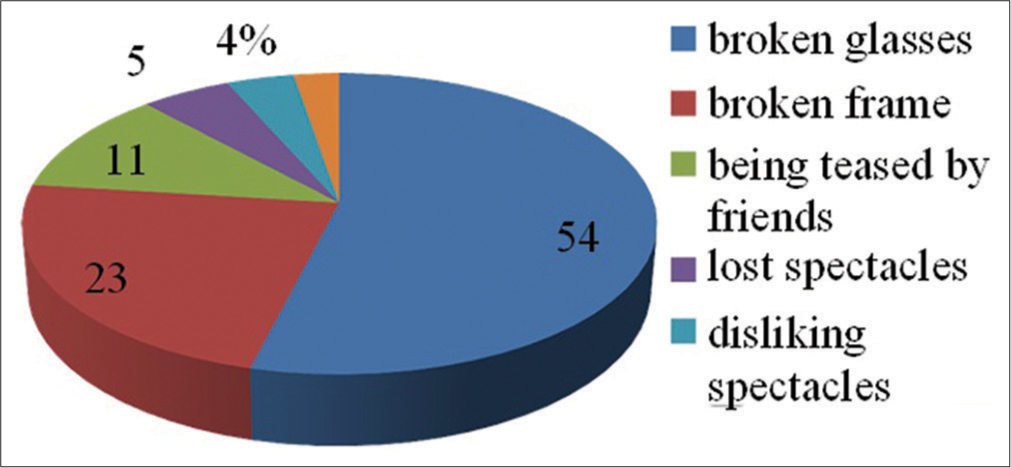
- Various reasons given by children for not using spectacles.
| VA | % Compliance |
|---|---|
| ≤6/12 Monocular | 32.85% (23 out of 70 children) |
| ≤6/12 Binocular | 61.30% (122 out of 199 children) |
VA: Visual acuity
DISCUSSION
Refractive errors are the most common cause of preventable blindness in school-going children in India.[2] The problem can easily be treated with spectacles, which is a quick and inexpensive option for treating refractive error. However, refractive errors go undetected in many children. School screening and spectacle distribution is a very good initiative taken by the government of India as recommended by the WHO. For that, the government of India is running school screening programs. However, in a country like India, with a huge population, the resources are limited. In previous reports, it has been emphasised multiple times that the coverage of school screening is not 100%,[6] and out of those screened, not all students receive spectacles even though prescribed. Even after spectacles are dispensed, the compliance level is very low, <50% in most former studies.[3,6,7] In the present study, the overall compliance to spectacle wear is 50.02%; this means that valuable resources (time, effort, energy, money and workforce) are getting wasted due to such poor compliance levels; this warrants the screening systems to be very efficient in terms of sensitivity and specificity. The resources should be used judiciously, meaning those who are likely to comply and benefit the most should be given priority. Furthermore, efforts should be made to identify the barriers and designated attempts should be made to increase the compliance levels. Ensuring the validity of a vision test for children is crucial to accurately identify those who will benefit from treatment, such as spectacles. The goal is to maximise the test’s sensitivity and specificity to avoid both false positives and false negatives. Using a visual acuity cutoff of < 6/6 in either eye can result in high sensitivity, meaning most children with visual impairment will be identified. However, this can also lead to a high number of false positives, causing unnecessary referrals and anxiety. The key is to find an optimal balance between sensitivity and specificity, ensuring that the test accurately identifies children who need treatment without overburdening healthcare services or causing undue stress to families.
It was seen that compliance dropped substantially when small degrees of refractive error were also prescribed glasses.[6] In our study, compliance was significantly better in children with unaided visual acuity ≤6/12 (53.90%) as compared to those with unaided visual acuity >6/12 (34.37%) (6/6 and 6/9). And even in those with ≤6/12, children with bilateral visual acuity ≤6/12, the compliance was better (61.30%) as compared to those with unilateral ≤6/12 (32.85%); this means that the children with better unaided visual acuity (UVA) in one eye were less likely to comply as compared to those with bilateral poor UVA. The observation shows that if the cutoff criteria are changed to ≤6/12, then better compliance is likely to ensue. Similar recommendations were there in a few other studies.[8] In other studies published in China,[9,10] India[7] and Mexico,[11] boys were less compliant to spectacle wear as compared to girls. However, we have found almost equal compliance levels in boys (49.32%) and girls (50.81%). The data observed can be partly due to the ‘cosmetic stigma’ prevalent in the region, associated with the spectacle wear: preventing girls from wearing them; so, the compliance becomes almost equal for boys and girls in contrast to previous studies reporting more compliance in girls pertaining to more ‘studious’ appearance being acceptable to girls more than boys.
Older children were more compliant with spectacle use (71.42%) as compared to younger children (39.06%); this is at par with the reports from other similar studies.[6,8] This is probably due to the understanding level of older children. In younger children, in whom refraction is a lot more difficult than older children, compliance is also low. They tend not to understand the significance and are likely to lose or break the frame frequently. For younger children, involving parents in the screening process and in purchasing spectacles could improve compliance. Furthermore, taking a guardian to the store to buy new glasses or checking the ill-fitted ones could help with the counselling for careful use and what not to do in caring for a child with glasses. For example, a lot of children benefitted from the idea of letting them choose the colour and shape of glasses, no matter how limited the choices were.
Being confident about wearing glasses is important as there often arises stigma[12,13] in the school environment as other children make fun of students wearing glasses; this could be avoided by positive reinforcement from the teachers. Appreciation from authoritative figures is often an important factor.
Counselling on certain factors, such as regular cleaning of glasses, ensuring proper storage, choosing a well-fitting frame and overcoming social stigma, should be kept in mind while explaining to the guardian.
Ease of reach to a spectacle dispensing centre had a positive correlation to compliance with the spectacle in many other studies[6] but it did not show any significant difference in our study; this was probably because most children got spectacle dispensing centres within 5–20 km range, which is still an easily reachable distance. If the distance is more, for example, 50– 100 km, then it would be very difficult to access. In our study, only three students were >20 km away from the spectacle dispensing centre. Hence, the distance has not significantly affected the compliance in our study. Spectacle distribution centres should be made reachable to up to 20 km or should be provided to the students in their respective schools to ensure more coverage.
During this study, it was also observed that some students who came for check-ups were looking for a new free pair of spectacles. In a few other studies, charging a token amount to the parents had a positive impact on the overall compliance level[12], as the parents would care for the spectacle more if they had paid even a small token amount. Furthermore, even though a few of them might be having a spectacle, they would say that they do not have one or lost/broken the same in the hope of getting a new free spectacle. This kind of behaviour indicates that the concept of everything being provided free of cost by the government needs to be revised. The government can implement a very small token amount to be charged to the parents to get them to value the resources, thus increasing the compliance level.
As we know, children are not small adults, and keeping a standard design[14,15] of spectacles that are unattractive to students reduces their compliance. Keeping a few variations in designs and colour or spectacle frames that not only look attractive but ensure a good centration will increase compliance.
Children spend their maximum time in school after home. Hence, appreciation of students who are wearing spectacles will create positive reinforcement and encourage them to wear spectacles. It will reduce the sense of an inferiority complex and the feeling that wearing spectacles is a disability.
A 3–6 monthly surprise visit to the school should be conducted by ophthalmic assistants to ensure compliance and counselling regarding regular cleaning and maintenance of spectacles to avoid scratches.
One of the limitations of our study was the inability to correlate parental education to compliance. The data could not be collected regarding the above as we had to rely on the answers of children.
Limitations of the study
Small sample size
Rather than relying on children’s answers, a surprise visit and observation by the investigating team would make the answers more reliable.
There was an observation that the children expected free spectacles from the field workers, so they were giving false answers to get the new pair of specs.
The reliability of answers in such cases becomes questionable.
Recommendations
Enhanced screening programs
Involve parents in screening processes and spectacle purchases
Ensure comprehensive and accurate prescriptions, avoiding minor refractive errors
In a country like India, with limited resources, the visual acuity cutoff for refraction in school children can be changed to 6/12 instead of 6/9 if the resources are limited; this will save a huge amount of energy, effort and resources spent on refraction and provision of spectacles.
Parental involvement and counselling
Educate parents on the importance of regular check-ups and proper spectacle maintenance.
Allow children to choose their frames to increase satisfaction and compliance.
Accessibility improvements
Ensure spectacle dispensing centres are within 5 kilometres or provide spectacles at schools.
Cost Sharing
Implement a policy where guardians bear a minimal cost for spectacles to foster responsibility.
Design and aesthetic considerations:
Offer a variety of attractive and well-fitting frames suitable for children.
School environment and reinforcement
Encourage teachers to reinforce spectacle use positively
Conduct regular follow-ups and counselling sessions to ensure ongoing compliance and proper maintenance.
CONCLUSION
Compliance with spectacle wear among school children in rural south Gujarat is suboptimal, with only 50.2% of students adhering to their prescribed use. Key factors influencing compliance include visual acuity, age and possibly the aesthetic appeal of the spectacles. Interventions to improve compliance should include enhanced screening programs, greater parental involvement and education, improved accessibility to spectacles, cost-sharing strategies and efforts to reduce the social stigma associated with wearing glasses. By addressing these multifaceted issues, it is possible to significantly improve compliance rates, ensuring better visual health and academic performance among children; this, in turn, represents a valuable investment in the future well-being and productivity of the population.
Ethical approval
The research/study was approved by the Institutional Ethics Committee at Divyajyoti Trust Tejas Eye Hospital, number ECR/942/Inst/GJ/2017, dated 20th October 2018.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Available from: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment [Last accessed on 2024 Jul 03]
- Refractive error in children in a rural population in India. Invest Ophthalmol Vis Sci. 2002;43:615-22.
- [Google Scholar]
- Prevalence of refractive errors among school-going children in a multistate study in India. Br J Ophthalmol. 2024;108:143-51.
- [CrossRef] [Google Scholar]
- Vision 2020 action plan 2006-2011. The International Agency for the Prevention of Blindness. Available from: https://www.iapb.org/learn/resources/vision-2020-action-plan-2006-2011 [Last accessed on 2024 Jul 02]
- [Google Scholar]
- Compliance to spectacle use in children with refractive errors-a systematic review and meta-analysis. BMC Ophthalmol. 2020;20:71.
- [CrossRef] [Google Scholar]
- Compliance of spectacle wear among school children. Indian J Ophthalmol. 2021;69:1376.
- [CrossRef] [Google Scholar]
- Spectacle compliance amongst school children of Rohtak, Haryana, India. Int J Community Med Public Health. 2017;4:734-7.
- [CrossRef] [Google Scholar]
- Vision testing for refractive errors in schools: Screening programmes in schools. Community Eye Health. 2000;13:3-5.
- [Google Scholar]
- Prevalence and determinants of spectacle non-wear among rural Chinese secondary schoolchildren: The Xichang Pediatric Refractive Error Study Report 3. Arch Ophthalmol. 2008;126:1717-23.
- [CrossRef] [Google Scholar]
- Need and challenges of refractive correction in urban Chinese school children. Optom Vis Sci. 2005;82:229-34.
- [CrossRef] [Google Scholar]
- Factors associated with spectacle-wear compliance in school-aged Mexican children. Invest Ophthalmol Vis Sci. 2006;47:925-8.
- [CrossRef] [Google Scholar]
- Barriers to spectacle use in Tanzanian secondary school students. Ophthalmic Epidemiol. 2008;15:410-7.
- [CrossRef] [Google Scholar]
- Spectacle adherence and barriers towards spectacle wear among primary school going children. Int J Res Med Sci. 2023;11:967-70.
- [CrossRef] [Google Scholar]
- Non-compliance of spectacle wear in school-going children with refractive errors. Cureus. 2024;16:e52702.
- [CrossRef] [Google Scholar]
- Compliance with spectacle wear and its determinants in school students in Central India. Asian J Ophthalmol. 2008;10:174-7.
- [Google Scholar]







