Translate this page into:
Bilateral cataract monovision surgery in a 54-year-old woman following Presbyond laser-blended vision: A case report
*Corresponding author: Linto Mathew Thomas, Department of Phaco and Refractive Surgery, Nethradhama Superspeciality Eye Hospital, Bengaluru, Karnataka, India. lintomathewthomas@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pereira SS, Thomas LM, Sriganesh S, Ganesh S. Bilateral cataract monovision surgery in a 54-year-old woman following Presbyond laser-blended vision: A case report. Glob J Cataract Surg Res Ophthalmol. doi: 10.25259/GJCSRO_47_2024
Abstract
This case report describes the feasibility of achieving spectacle independence after cataract surgery in a patient who has undergone Presbyond laser-blended vision (LBV) for presbyopia correction 5 years back. A 54-year-old woman presented with a gradual diminution of vision in both eyes for 2 years. On examination, unaided distance visual acuity (UDVA) was 20/40 in oculus uterque (OU), and corrected distance visual acuity (CDVA) was 20/40, N5 binocularly. The primary diagnosis was posterior subcapsular cataract with nuclear sclerosis grade 1 with status post-Presbyond LBV. Cataract surgery with aspheric monofocal intraocular lens (IOL) and monovision by targeting dominant oculus dexter (OD) to emmetropia and non-dominant oculus sinister (OS) to myopia of –1.5 D was planned for the patient. Multiple formulae were used to calculate the IOL power and it was decided to implant + 24.0 D in OD and + 22.5 D in OS calculated using Barrett’s True K TK/TK universal II formula. At post-operative day 15, no complications were noted, UDVA in OD was 20/20 and in OS was 20/125 and CDVA was 20/20 in OS. Uncorrected near visual acuity was N10 in OD and N5 in OS, with a refraction of –1.75DS/–0.50DC @15 degrees in OS (Monovision) which was stable even at 6 months follow-up. The patient achieved good distance, intermediate and near vision due to the pre-existing corneal spherical aberrations induced by Presbyond. The choice of aspheric IOL with appropriate power prevented change in the total spherical aberrations and helped to achieve spectacle independence in this patient.
Keywords
Cataract surgery
Monovision
Presbyond
INTRODUCTION
Presbyond laser-blended vision (LBV) is a presbyopia treatment option from Zeiss (Carl Zeiss Meditec, Germany) which uses a combination of monovision and induction of spherical aberration, which leads to an increase in the depth of focus. This results in spectacle independence binocularly for all distances.[1]
These patients eventually require cataract surgery and care should be taken so that the benefit of LBV induced by Presbyond is carried forward after cataract surgery by preserving the induced spherical aberrations. This will ensure that the patient will continue to remain spectacle-independent at distance, intermediate and near vision binocularly.
CASE REPORT
A 54-year-old woman presented with a gradual diminution of vision in both eyes for 2 years. She gives a history of undergoing Presbyond LBV 5 years back. Unaided distance visual acuity was 20/40 OU with no improvement and uncorrected near visual acuity was N18 in OD and N5 in OS, binocularly reading N5. Measurement of visual acuity was done using early treatment diabetic retinopathy study (ETDRS) charts (Precision Vision, La Sella, IL, USA). OD was dominant. Intraocular pressures recorded with non-contact tonometry (NCT) (Tomey NCT, NishiKu, Nagoya, Japan) was 12 mm Hg in both eyes. A gonioscopy revealed open angles in both eyes. The Z (4.0) of spherical aberration in OD was −0.613 um, and in OS, it was 0.483 um.
On examination, the patient was orthophoric on a cover test, extraocular movements were full and free and with a well-dilating pupil in both eyes (8 mm). Corneal topography (Pentacam HR, Oculus, Wetzlar, Germany) revealed K1: 44.30 D, K2: 44.80 D in OD and K1: 46.4, K2: 47.0 D in OS with myopic pattern post refractive surgery topography. Anterior chamber depth was 3.5 mm OD, 3.68 mm OS. White-to-white measurement was 12.6 mm OD and 12.7 mm in OS, measured using Scheimpflug technology (Pentacam HR, Oculus, Wetzlar, Germany) [Figure 1]. On examination of the anterior segment, both eyes’ cornea showed a clear interface with an 8 mm Femto Lasik scar, with posterior subcapsular cataract and nuclear sclerosis grade 1. A dilated fundus examination revealed normal fundus. Keeping her previous corneal procedure in mind, a monovision cataract surgery with an aspheric intraocular lens (IOL) was planned to achieve vision for near, intermediate, and distance and not to induce new aberrations.
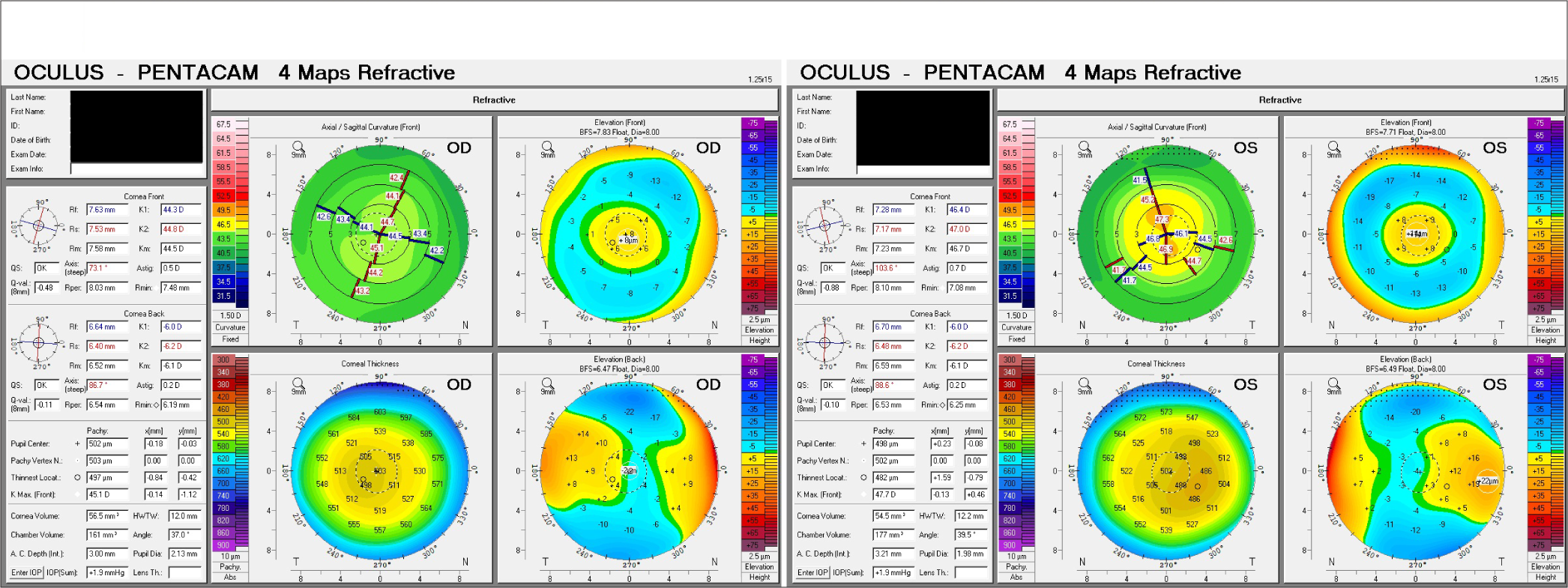
- Pre-operative Scheimpflug imaging showing corneal topography after Presbyond in the right eye and left eye. OD: Oculus dexter, OS: Oculus sinister.
IOL power calculations were done using optical biometry (IOL Master 700-Carl Zeiss Meditec, Jena, Germany). Formulae used were – Barrett’s TK Universal II, Barrett’s True-K, Barrett’s True-K total keratometry (TK), Haigis-L, Holladay-2 with equivalent keratometry reading (EKR) and ray trace, which gave variable refractive outcomes. The IOL power calculated by Barrett TK Universal II/Barrett’s True-K TK was used.[2] The IOL power was +24.0 D in OD and +22.50 D in OS. A monofocal aspheric IOL was used (Zeiss CT Lucia 621) [Table 1]. OS was operated first followed by OD. Routine phacoemulsification surgery was done using a 2.8 mm incision. The procedure was uneventful for both eyes. At postoperative day 15, no complications were noted. Binocularly, the patient maintained a corrected distance visual acuity of 20/20 through the 6-month follow-up period [Table 2].
| Formula | Right Eye | Left Eye | ||
|---|---|---|---|---|
| IOL power | Residual power | IOL power | Residual power | |
| Barrett’s TK | +24.00 | −0.24 | +22.50 | −1.44 |
| Barrett’s True-K | +24.50 | +0.02 | +23.00 | −1.55 |
| Barrett’s True K TK | +24.00 | +0.06 | +22.50 | −1.37 |
| Holladay 2 with EKR | +23.5 | −0.10 | +22.50 | −1.49 |
| Haigis-L | +25.5 | +0.06 | +24.50 | −1.56 |
| Raytrace | +24.00 | +0.04 | +22.00 | −1.38 |
IOL: Intraocular lens, TK: Total keratometry, EKR: Equivalent keratometry reading
| Parameters | Right Eye | Left eye | ||||
|---|---|---|---|---|---|---|
| Pre-operative | POD-15 | POD-6 months | Pre-operative | POD-15 | POD-6 months | |
| Sph (D) | NI | −0.25 | −0.25 | NI | −1.75 | −1.50 |
| Cyl (D) | NI | −0.25 | −0.25 | NI | −0.5 | −0.75 |
| Axis | 110 | 125 | 15 | 180 | ||
| UDVA | 20/40 | 20/20 | 20/20 | 20/40 | 20/125 | 20/80 |
| CDVA | 20/40 | 20/20 | 20/20 | 20/40 | 20/20 | 20/20 |
| UNVA | N18 | N10 | N10 | N5 | N5 | N5 |
| CNVA (+2.00D) | N5 | N5 | N5 | |||
| Pre-operative | POD- 15 | POD-6 months | ||||
| Binocular UDVA | 20/40 | 20/20 | 20/20 | |||
| Binocular UNVA | N5 | N5 | N5 | |||
UDVA: Unaided distance visual acuity, UNVA: Uncorrected near visual acuity, CDVA: Corrected distance visual acuity, POD: Post operative day, Sph: Sphere, Cyl: Cylinder, CNVA: Corrected near visual acuity
Binocular defocus curves were plotted with distance correction from + 3.00 to − 3.00 D. The curve showed two peaks at −0.50 D and +0.5D, corresponding to a visual acuity of 0.0 logarithm of the minimum angle of resolution (logMAR), followed by a gradual decline. A mean visual acuity of 0.0 log MAR or better was observed within the defocus range of −0.5 to + 0.50 D, and a full range of functional vision, that is, 0.2 logMAR (20/30) or better, was achieved from + 0.50 to −1.00 D of defocus [Figure 2].
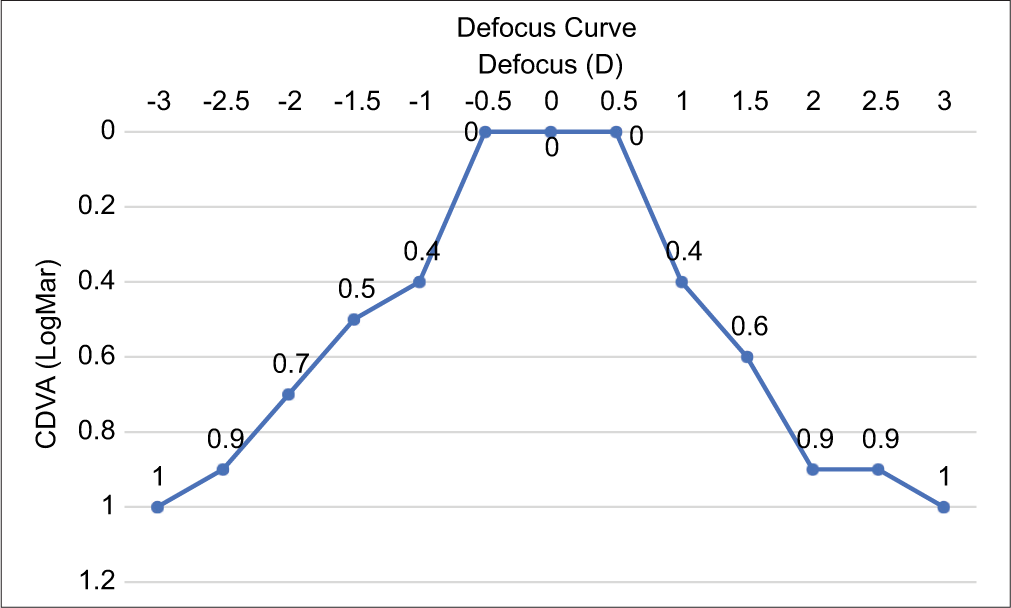
- Defocus curve. CDVA: Corrected distance visual acuity.
Using the Salzburg reading desk, the patient’s reading performance was evaluated. She was able to read 162 words/min at a distance of 40 cm and 164 words/min at 66 cm, signifying a comfortable reading at both 40 and 66 cm post-monovision cataract surgery.
DISCUSSION
Surgical correction of presbyopia with Presbyond is an advanced technique used by refractive surgeons worldwide. This patient has been comfortable with LBV for 5 years; therefore, the same design of cataract surgery should be taken into consideration.
In this case, we have used the Barrett TK/True-K TK formula which was more accurate compared to other popular post-refractive surgery formulas. It has been improved using historical data and measured posterior corneal power.[3-5]
With the use of aspheric monofocal IOLs to retain the Presbyond ‘blended vision’, not only are the photopic phenomena associated with multifocal IOLs minimised, but a larger number of patients can be considered as potential candidates.[6] EDOF IOLs are not suitable for patients with a history of Presbyond as they induce spherical aberrations. This will no longer have the benefit of the induced spherical aberrations by Presbyond, causing a drop in visual acuity. A potential disadvantage is a decrease in retinal image quality if the amount of aberrations is excessively increased.[7]
CONCLUSION
The technique of monovision has been in use for years, whether with contact lenses, corneal refractive surgery or pseudophakia. In this case, it helped the patient in achieving near-, intermediate-, and distant vision without any spectacles. Since this patient had already undergone a corneal refractive procedure using the LBV technique, doing cataract surgery using monofocal aspheric IOL, which does not induce spherical aberration, was found feasible and accurate than any other lenses achieving good intermediate vision along with good distance and near vision. Appropriate IOL power calculation formula for the calculation of lens power should be used in such cases status post-refractive surgery. In this case, it was achieved using Barrett’s TK universal II/True-K TK formula.
Author’s contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICJME) criteria for authorship.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- LASIK for presbyopia correction in emmetropic patients using aspheric ablation profiles and a micro-monovision protocol with the Carl Zeiss Meditec MEL 80 and VisuMax. J Refractive Surg. 2012;28:531-41.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of intraocular lens power prediction methods using the American society of cataract and refractive surgeons post-keratorefractive intraocular lens power calculator. J Cataract Refract Surg. 2010;36:1466-73.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular lens calculation after refractive surgery for myopia: Haigis-l formula. J Cataract Refract Surg. 2008;34:1658-63.
- [CrossRef] [PubMed] [Google Scholar]
- Intraocular lens power calculation following laser refractive surgery. Eye Vis (Lond). 2015;2:7.
- [CrossRef] [PubMed] [Google Scholar]
- IOL power calculations after LASIK or PRK: Barrett True-K biometer-only calculation strategy yields equivalent outcomes as a multiple formula approach. J Cataract Refract Surg. 2022;48:784-9.
- [CrossRef] [PubMed] [Google Scholar]
- Reading ability with pseudophakic monovision and with refractive multifocal intraocular lenses: Comparative study. J Cataract Refract Surg. 2009;35:1501-4.
- [CrossRef] [PubMed] [Google Scholar]
- Extended depth-of-field intraocular lenses: An update. Asia Pac J Ophthalmol (Phila). 2020;9:194-202.
- [CrossRef] [PubMed] [Google Scholar]







