Translate this page into:
Foveolitis with fever: An optical tomography biomarker for dengue maculopathy
*Corresponding author: Deepak Narain Bhojwani, Department of Vitreo Retina, Bhojwani Eye Hospital Retina Center, Ahmedabad, Gujarat, India. bhojwani.deepak1986@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bhojwani DN. Foveolitis with fever: An optical tomography biomarker for dengue maculopathy. Glob J Cataract Surg Res Ophthalmol. 2024;3:79-81. doi: 10.25259/GJCSRO_4_2024
Abstract
We report a case of a 25-year-old boy presenting to an ophthalmologist with unilateral foveolitis associated with fever. After a thorough ocular clinical examination and with the aid of the characteristic finding of foveolitis on optical coherence tomography, a probable clinical diagnosis of dengue fever maculopathy secondary to systemic dengue was made. The patient was referred to the physician for systemic management of dengue. On laboratory investigation, the patient was found to be seropositive for dengue virus. The patient was treated with topical and systemic steroids from our end besides receiving general symptomatic care at the physician’s end. This case highlights the role of an ophthalmologist in promptly diagnosing and managing dengue-related ocular complications in collaboration with a physician.
Keywords
Dengue maculopathy
Foveolitis
Optical coherence tomography
INTRODUCTION
Dengue fever is a common endemic disease in India caused by Flavivirus and transmitted by Aedes mosquitos.[1] Dengue maculopathy is the most common reported ocular manifestation and its prevalence is reported to be around 10% among hospitalised patients.[2] The most common presenting ocular symptoms reported with dengue maculopathy are blurry vision, scotoma, ocular pain, and metamorphopsia. The pathophysiology of dengue maculopathy is presumed to be driven by immune-complex-mediated processes.[3]
CASE REPORT
A 25-year-old boy presented to us with a sudden painless blurring of vision in his right eye for the past 1 week. On detailed enquiry, he also gave a history of fever associated with arthralgia and myalgia 10 days before experiencing visual symptoms. He was taking over-the-counter antipyretic and analgesic medications for the same.
On ocular examination, the visual acuity in the right eye was 6/12 N18 and 6/6 N6 in the left eye. Anterior segment examination was unremarkable in both eyes. Fundus examination of the right eye revealed multiple focal ill-defined yellowish subretinal patches associated with retinal oedema centered on the posterior pole associated with vitreous haze along with a few superficial retinal haemorrhages and venous tortuosity [Figure 1a]. Left eye fundus examination was within normal limits. Optical coherence tomography (OCT) of the right eye had a classic picture of foveolitis with focal disruption of outer retinal layers, and hyperreflective conical elevation associated with few parafoveal cystic spaces [Figure 1b].
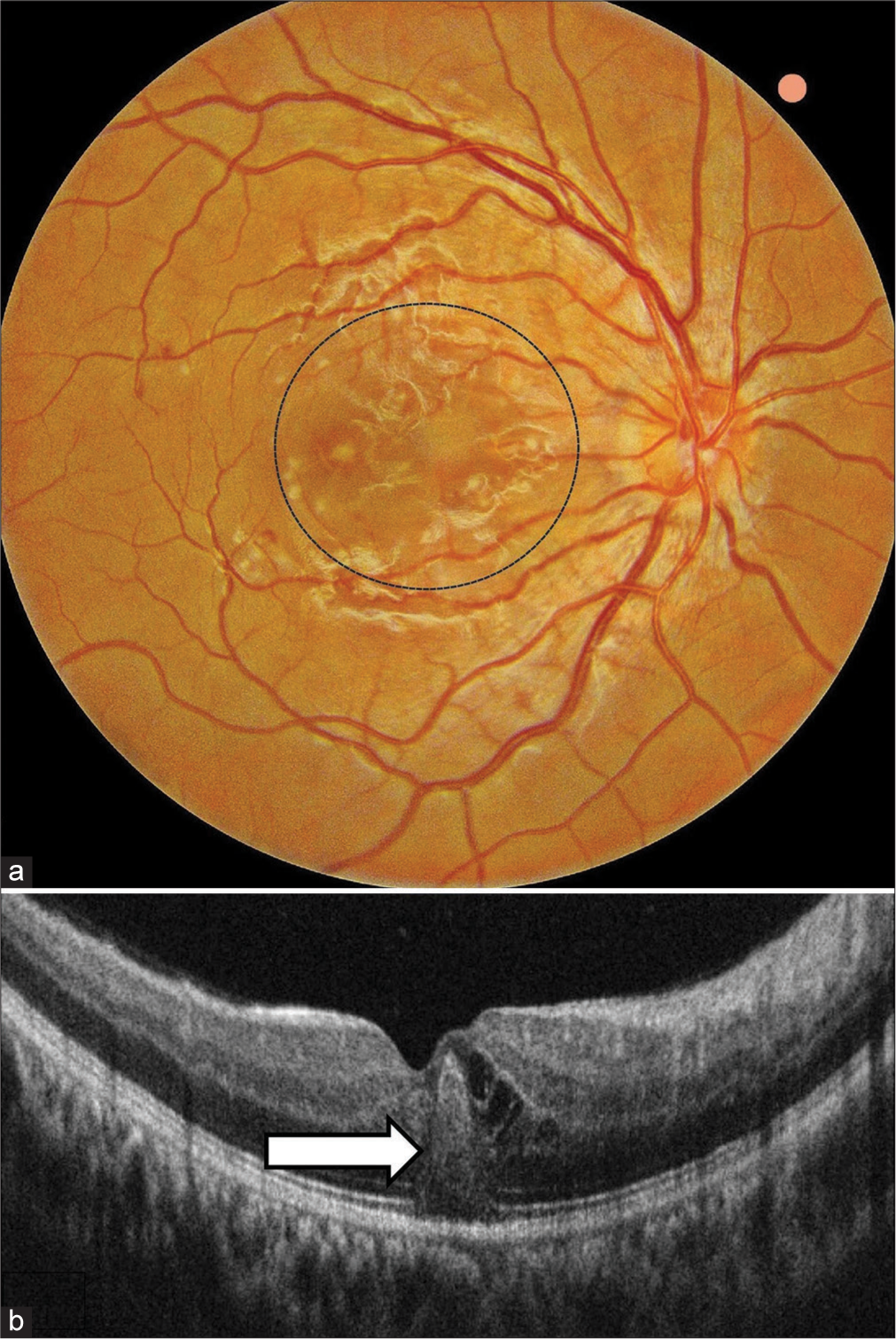
- (a) Colour fundus photograph of the right eye showing multiple focal ill-defined yellowish subretinal patches associated with retinal oedema centred on the posterior pole (circle) associated with few superficial retinal haemorrhages and venous tortuosity. (b) Optical coherence tomography documenting classic foveolitic picture (arrow) with conical protrusion of hyperreflective material in outer retina along with cystoid swelling in inner retinal layers.
On collaborating the clinical history, fundus findings, and characteristic foveolitis sign on OCT, a provisional clinical diagnosis of dengue-associated maculopathy was made secondary to systemic dengue.
The patient was referred to a physician for the same and was found to be seropositive for dengue virus non-structural protein1 and Immunoglobulin M (IgM) antibody. Furthermore, the haematological parameters of the patient, especially platelet counts, were found to be reduced (68,000/μL) supporting systemic dengue disease. The patient was started on systemic steroids (40 mg) along with general symptomatic care by the physician.
At a 2-week follow-up, the visual acuity of the right eye improved to 6/6 N6, and foveal architecture was also restored on OCT [Figure 2]. The patient’s systemic parameters were also found to be within normal range during his follow-up visit. The patient was maintaining 6/6 vision with normal fundus findings in both eyes at his 3-month follow-up visit with us.

- (a) Post-treatment fundus photograph showing resolution of dengue maculopathy. (b) Optical coherence tomography documenting complete restoration of foveal structure with intact external limiting membrane and outer retinal layers.
DISCUSSION
The ocular features of dengue maculopathy usually manifest within 10 days of the onset of fever.[4] This delay in the manifestation of ocular symptoms from the onset of systemic dengue fever supports the theory of immune-mediated pathophysiology rather than direct viral infection. More than a week symptom-free interval usually corresponds to the time of onset of the immunological response of antibody production, immune complex deposition, or production of autoantibodies.
Dengue foveolitis refers to a disruption of the outer neurosensory retina in OCT and is clinically seen as yellow-orange lesions in the foveal area.[5] Agarwal, et al. have demonstrated foveolitis as a conical foveal elevation with disruption of outer retinal layers on swept-source OCT in their study and have attributed it secondary to ischaemic and inflammatory components.[6]
OCT is an important diagnostic tool in monitoring the severity of dengue-associated maculopathy. Teoh et al.[7] have reported three patterns on OCT in dengue maculopathy which include type 1 (diffuse retinal thickening; 44.6%), type 2 (cystoid macular oedema; 21.6%), and type 3 (foveolitis; 33.8%). Diffuse retinal thickening in OCT was associated with the best prognosis, and the foveolitis group was associated with the poorest prognosis in their study. Although our patient had a type 3 foveolitis pattern on presentation, he recovered satisfactorily with treatment without any residual scotomas or visual deficits.
The majority of the patients with dengue-associated ocular disease have a self-limiting course and resolve spontaneously. Both systemic and topical steroids are found to be effective in symptomatic patients with decreased vision because of dengue-associated ocular complications.[8] Our patient also responded remarkably well to treatment with topical and systemic steroids.
Our patient is a rare case event where the patient reported to an ophthalmologist with ocular symptoms. The ophthalmologist diagnosed the patient with dengue maculopathy based on classical foveolitis sign on OCT. The clinical diagnosis was confirmed through serological investigations and collaborative support from a physician. Gupta et al. have also reported three cases who first presented to an ophthalmologist with a diminution of vision and a pre-existing history of fever and constitutional symptoms. All three cases were later diagnosed to be serologically positive for dengue virus.[9] It is interesting to note that the foveolitis sign on OCT has been commonly reported only with dengue maculopathy among all other causes of post-fever retinitis diseases.[10].
CONCLUSION
We believe that in any patient presenting with ocular symptoms with a pre-existing history of fever along with constitutional symptoms, the OCT finding of foveolitis can be a diagnostic pointer to underlying systemic dengue disease.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of Interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Prevalence of dengue maculopathy in patients hospitalized for dengue fever. Ophthalmology. 2007;114:1743-7.
- [CrossRef] [PubMed] [Google Scholar]
- Dengue-associated maculopathy. Arch Ophthalmol. 2007;125:501-10.
- [CrossRef] [PubMed] [Google Scholar]
- Ophthalmic complications of dengue fever: A systematic review. Ophthalmol Ther. 2012;1:2.
- [CrossRef] [PubMed] [Google Scholar]
- Dengue-induced inflammatory, ischemic foveolitis and outer maculopathy: A swept-source imaging evaluation. Ophthalmol Retina. 2019;3:170-7.
- [CrossRef] [PubMed] [Google Scholar]
- Optical coherence tomography patterns as predictors of visual outcome in dengue-related maculopathy. Retina. 2010;30:390-8.
- [CrossRef] [PubMed] [Google Scholar]
- Dengue fever presenting with macular hemorrhages. Retina Cases Brief Rep. 2011;5:213-8.
- [CrossRef] [PubMed] [Google Scholar]
- Post-fever retinitis-newer concepts. Indian J Ophthalmol. 2020;68:1775-86.
- [CrossRef] [PubMed] [Google Scholar]






