Translate this page into:
Harmful traditional eye practices in Nigeria and its burden on eye care: A review of literature
-
Received: ,
Accepted: ,
How to cite this article: Nathaniel GI, Eze UA. Harmful traditional eye practices in Nigeria and its burden on eye care: A review of literature. Glob J Cataract Surg Res Ophthalmol. doi: 10.25259/GJCSRO_29_2023
Abstract
Background/Aim:
The use of traditional eye medication (TEM) is an age-long practice whose negative effects on eye health have been well documented. TEM involves the application of different harmful preparations to the eye as a form of treatment. This article is aimed at highlighting the burden of harmful traditional practices on eye care in Nigeria.
Methodology:
A review of available literature was conducted to summarize the different types of harmful traditional eye practices in Nigeria, including the many different preparations used. Prevalence of harmful traditional practices, determinants, burden in Nigeria. Issues relating to determinants, prevalence, indications for TEM use, presentation of patients with a history of TEM use, ocular complications following TEM use, the pathway to blindness with TEM use, economic burden, and prevention were considered in the review. The prevalence of TEM use was 15.5%, and the common determinants included low socioeconomic status, rural residence, poor access to conventional eye care, and cultural beliefs. The indications for the use of these medications included blurring of vision, red eyes, ocular pain, and itching. Patients who used TEMs presented with various levels of visual impairment (14.5% and 13.1%, respectively, for moderate and severe visual impairment), and 51.3% were reported blind at presentation. The common complications of these agents were corneal scars (opacities), staphylomas, endophthalmitis and panophthalmitis, corneal ulcers and perforations, uveitis, band and bullous keratopathies, complicated cataracts, subluxated lens, and descemetoceles.
Conclusion:
The prevalence of TEM use, visual impairment, and blindness arising from it is high in Nigeria. The ocular morbidities that follow TEM use constitute a significant burden (economic and otherwise) on eye care delivery in the country. A multipronged approach by stakeholders is required to mitigate the enablers of TEM practice in Nigeria. Furthermore, where there are complications, prompt referral to an ophthalmologist is advocated as they are well-equipped to provide the most appropriate management.
Keywords
Harmful traditional eye practices
Prevalence determinants
Burden
Nigeria
INTRODUCTION
According to the World Health Organization, traditional medicine (TM) is a combination of knowledge, skills, and practices used for health maintenance as well as in the prevention, diagnosis, treatment, or improvement of physical, mental, or social diseases based on theories, beliefs and past indigenous experience from cultures and handed down through generations in a verbal or written form.[1] The history of TM dates back to the Stone Age.[2]
Traditional eye medication (TEM) consists of practices or biologically based therapies, organic or inorganic agents that can be applied through different routes of administration to achieve a desired ocular therapeutic effect.[3] Traditional eye practices are defined as activities that include the use of TEM, performing sacred rituals and prayers, or ophthalmic self-medication to cure an ocular ailment.[4] Some of these practices involve the use of or application of substances or mechanical or thermal devices to eye surfaces and adnexa.[5] Common examples of such substances include seawater, contaminated water, dry gin, extracts of roots, leaves or trees, herbs, vegetables, powdered charcoal, breast milk, human urine and saliva, excreta of cattle and lizards, kerosene, petrol and other hydrocarbons.[5,6] These substances are either contaminated (due to poor hygiene handling an application) or toxic to tissues (acidic or alkaline in nature). While contamination exposes the ocular tissues to highly infectious organisms, which have devastating outcomes, toxic substances can result in corrosion of the affected tissues.
In most developing countries like Nigeria, alternative practice (TEM) is usually the first line of care as against orthodox or conventional care. The main reasons for this trend are affordability, accessibility, lack of awareness of other options, and perception that TEM is natural, which makes it better than conventional treatment, and, as a result, dissatisfaction with natural treatment.[6,7] Often, the consequences of these practices culminate in avoidable blindness as these conditions could otherwise have been managed easily without complications and ocular morbidities. Conversely, it is important to note that face washing with clean water, which is a traditional practice, is a documented and accepted strategy for the control of trachoma.[8]
This review aims to highlight the burden of harmful traditional practices on eye care in Nigeria.
METHODS
This was a traditional narrative review. A Google search was conducted using the Medical Subject heading such as prevalence of harmful traditional practices, determinants, burden, Nigeria. Information obtained was summarised as determinants, prevalence, indications for TEM use, presentation of patients with a history of TEM use, ocular complications following TEM use, the pathway to blindness with TEM use, economic burden, and prevention.
DISCUSSION
Epidemiology
Determinants
In general, the factors that encourage TEM use include limited access to orthodox eye care – likely due to maldistribution of health facilities, especially in rural areas; cultural beliefs and practices, especially in the rural areas; economic factors and lack of awareness.[9,10] In addition, the heightened interest in the practice of TEM may be a possible factor.[11,12]
A study in Ekiadolor, a semi-urban community in Edo state, showed that over 90% of the study population were aware of 48.7% of patients with eye conditions in the previous year who used TEM against 41.4% who used orthodox medications.[7] The reasons given by the respondents of this study included affordability (21.8%), being unaware of orthodox medication (16.5%), preference for natural therapy (14.3%), unsatisfactory orthodox treatment (13.5%), and lack of access (9.8%). The same study reported that males were more likely to use TEM in the community (P < 0.001, odds ratio 2.13). Furthermore, low socioeconomic class was a significant determinant of TEM use (P < 0.001).[7] There was a significant association (P < 0.001) between educational status and the use of TEM, as those without formal education were 34.8 times more likely to use TEM compared to those with tertiary education.[7]
Prevalence
Over the years, different studies in Nigeria have reported different prevalence rates of TEM use in Nigeria. The prevalence varies from 1.6% to 55% from the different studies[3,4,11-14], and the average prevalence of TEM use in Nigeria is 15.5% [Table 1].
| Authors, year of publication | Location | Design | Prevalence | Nature of TEM (%) |
|---|---|---|---|---|
| Eze et al., 2009.[5] | Enugu, southeast Nigeria (Urban) | Comparative cross-sectional | 55% | Animal products Human urine–2.7 Human breast milk–1.3 Cod liver oil–0.7 Plant products herbal extract–28.2 Aloe vera product–6.7 Palm wine–1.3 Palm oil–0.7 Bitter kola extract–0.7 Chemical substances Holy water–37.6 Anointed oil/olive oil–8.7 Black stone–2.7 Natural (spring) water–2.0 Powder–1.3 Salt solution–1.3 Sugar solution–1.3 Forever living product–0.7 Antimony–0.7 Kerosene–0.7 Harcogen rub–0.7 |
| Ukponmwan and Momoh, 2010.[11] | Benin, south-south Nigeria | Prospective study | 1.6% | Plant extract–54.9 Concoction–21.2 Breast milk–3.5 Religious item–3.5 Lead antimony–1.8 Urine–1.8 Soot–0.9 Alcohol–0.9 Not known–11.5 |
| Nwosu and Obidiozor, 2011.[12] | Onitsha, southeast Nigeria (Urban) | Cross-sectional | 3.4% | Liquid (from leaves/roots)–86.4 Human urine–6.1 Sugar solution–3.0 Powdery substance–3.0 Holy water–1.5 |
| Ajite and Fadamiro, 2013.[13] | Ado Ekiti, southwest Nigeria (Urban) | Retrospective cross-sectional | 13.2% | Kerosene–33.3 Cassava water–20.8 Personal urine–14.6 Cow urine–8.3 Breast milk–8.3 Battery water–4.2 Brake fluid–4.2 Traditional Concoction–4.2 Onion–2.1 |
| Achigbu and Achigbu 2017.[14] | Owerri, southeast Nigeria (Urban) | Cross-sectional | 15.8% | - |
| Oyediji, et al., 2019.[3] | Mangu, north central Nigeria (rural/sub-urban) | Cross-sectional | 4.3% | Plant product Leaf extract–28.7 Roots–1.9 Dry leaves–6.7 Chemical powder–29.6 Eye pencil–3.7 Salt solution–0.9 Cigarette smoke 0.9 Animal products Human saliva–1.9 Human urine–0.9 Human breast milk–0.9 Cow milk–0.9 Other concoctions–6.5 Unknown–16.7 |
TEM: Traditional eye medication
INDICATIONS FOR USE OF TEM
There are different indications for the use of TEM in Nigeria, and the most common include blurring of vision, red eyes (inflammation), ocular pain, and itching [Figures 1 and 2].[10,13]
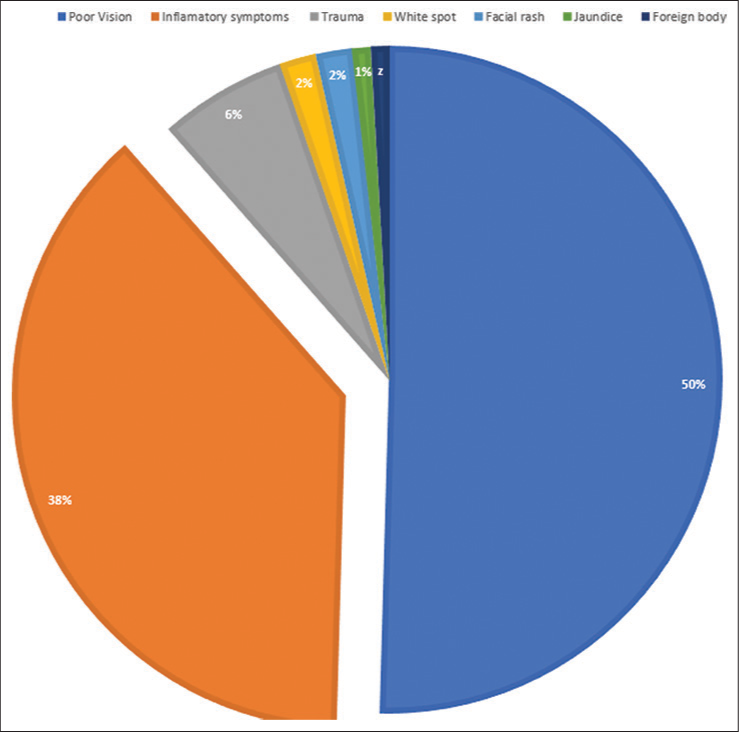
- Distribution of the ocular indication for traditional eye medication use in Benin (Ukponwan and Momoh, 2010).
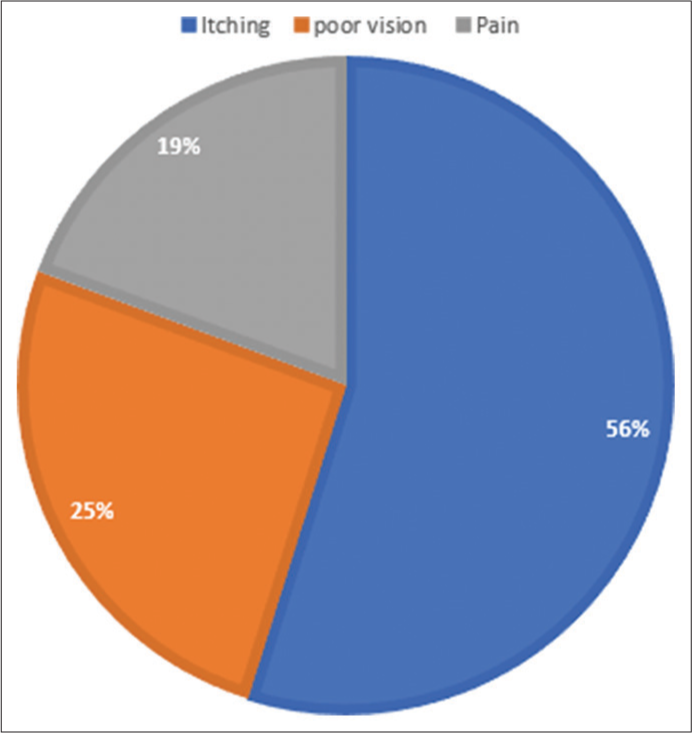
- Distribution of the ocular indication for traditional eye medication use at Owerri (Achigbu and Achigbu, 2017).
OCULAR PRESENTATIONS FOLLOWING USE OF TEM
The majority of patients who use TEM as first-line treatment usually presented to the hospital with complicated ocular conditions with varying degrees of visual impairment. In Benin City (2010), Ukponmwan and Momoh reported that 86% of such patients were legally blind in the affected eye at presentation. Meanwhile, 5.3%, 1.8%, and 7.1% presented with severe, moderate, and mild visual impairment, respectively.[11] In Enugu (2009), diminution of vision, itching, and discharge were the most common presenting symptoms following the use of TEM, with about a quarter of eyes blind at presentation.[3] However, the majority (80.5%) of the patients had discontinued the use of TEM at presentation due to poor response, worsening condition, and peer counsel.[3] Another report by Nwosu in southeast Nigeria showed that almost 40% of patients who presented late with penetrating eye injuries had used TEM before coming to the hospital.[15]
From available literature, the proportion of patients with a prior history of TEM use at presentation to hospital with normal vision to mild visual impairment was 21.3%, moderate visual impairment 14.5%, and severe visual impairment 13.1%, while the prevalence of blindness was 51.3% [Table 2].
| Proportion (%) | ||
|---|---|---|
| Ukponmwan and Momoh, Benin (2010)[11] | • Normal vision-mild visual impairment • Moderate visual impairment • Severe visual impairment • Blindness |
7.1 1.8 5.3 85.9 |
| Ajite and Fadamiro (2013)[13] | • Normal vision-mild visual impairment • Moderate visual impairment • Severe visual impairment • Blindness |
35.4 27.1 20.8 16.7 |
TEM: Traditional eye medication
COMMON OCULAR COMPLICATIONS OF USE OF TEM
Despite the repeated claim of TM practitioners that TEM can treat numerous conditions, available evidence suggests otherwise, as most initial users of TEM within and beyond Nigeria usually present with TEM-related ocular complications.[16] In a study to determine the incidence and complications of TEM in a Nigerian Teaching hospital, Ukponmwan and Momoh (Benin, 2010) reported that more than 50% of prior TEM users presented with ocular complications of varying frequencies.[11] These ocular complications included corneal scars (opacities) [Figure 3], staphylomas, endophthalmitis and panophthalmitis [Figure 4], corneal ulcers and perforations, uveitis, band and bullous keratopathy, complicated cataracts, subluxated lens, and descemetoceles. These resulted in either enucleation or evisceration of the affected eye.[11,15,16]
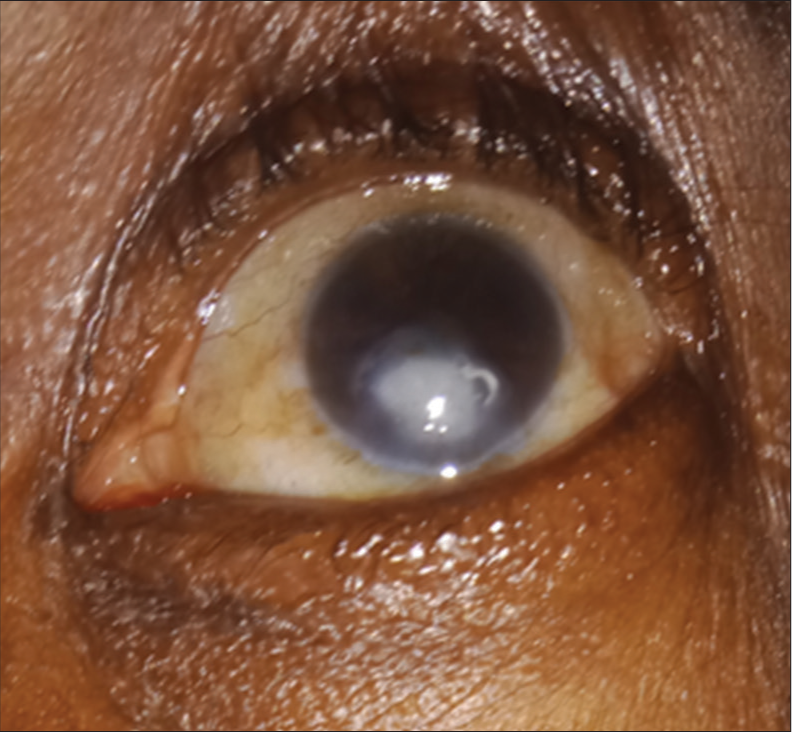
- Showing a patient with corneal opacity following traditional eye medication use for presumed measles infection in childhood (courtesy of Dr. U Eze).
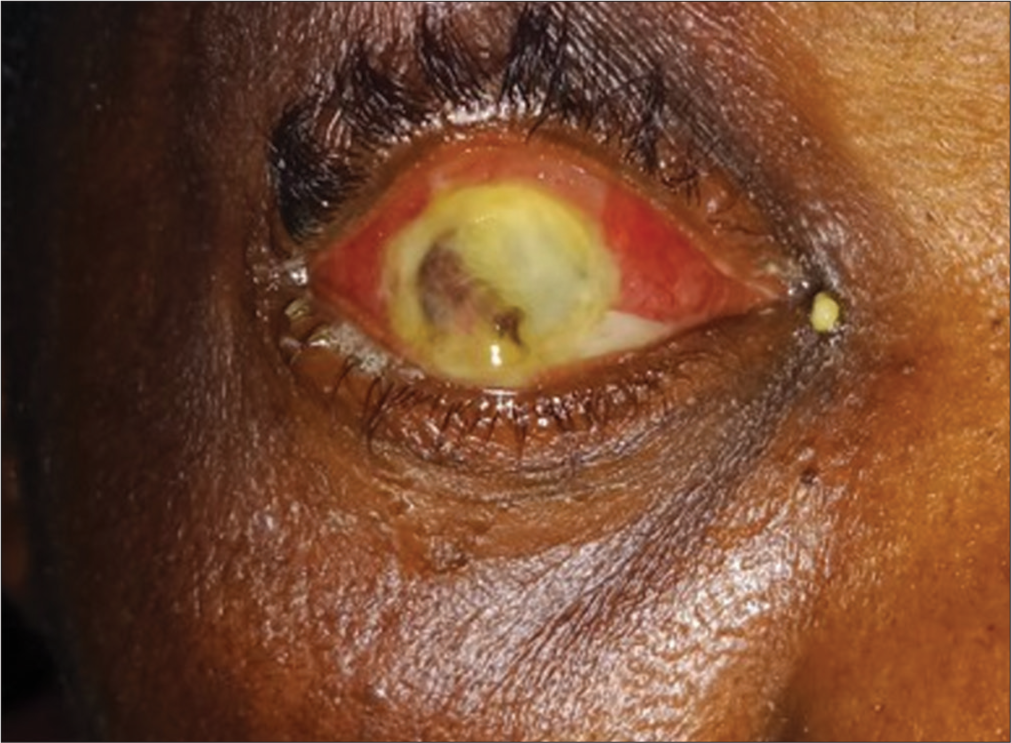
- Panophthalmitis in a patient with a history of steroid and traditional eye medication use (courtesy of Dr. U Eze).
MECHANISMS/PATHWAY TO BLINDNESS FROM TEM USE
The pathway to blindness from TEM use is complex and depends on the type of material contained in the TEM. [Figure 5] illustrates the multiple pathways to blindness associated with the use of TEM.
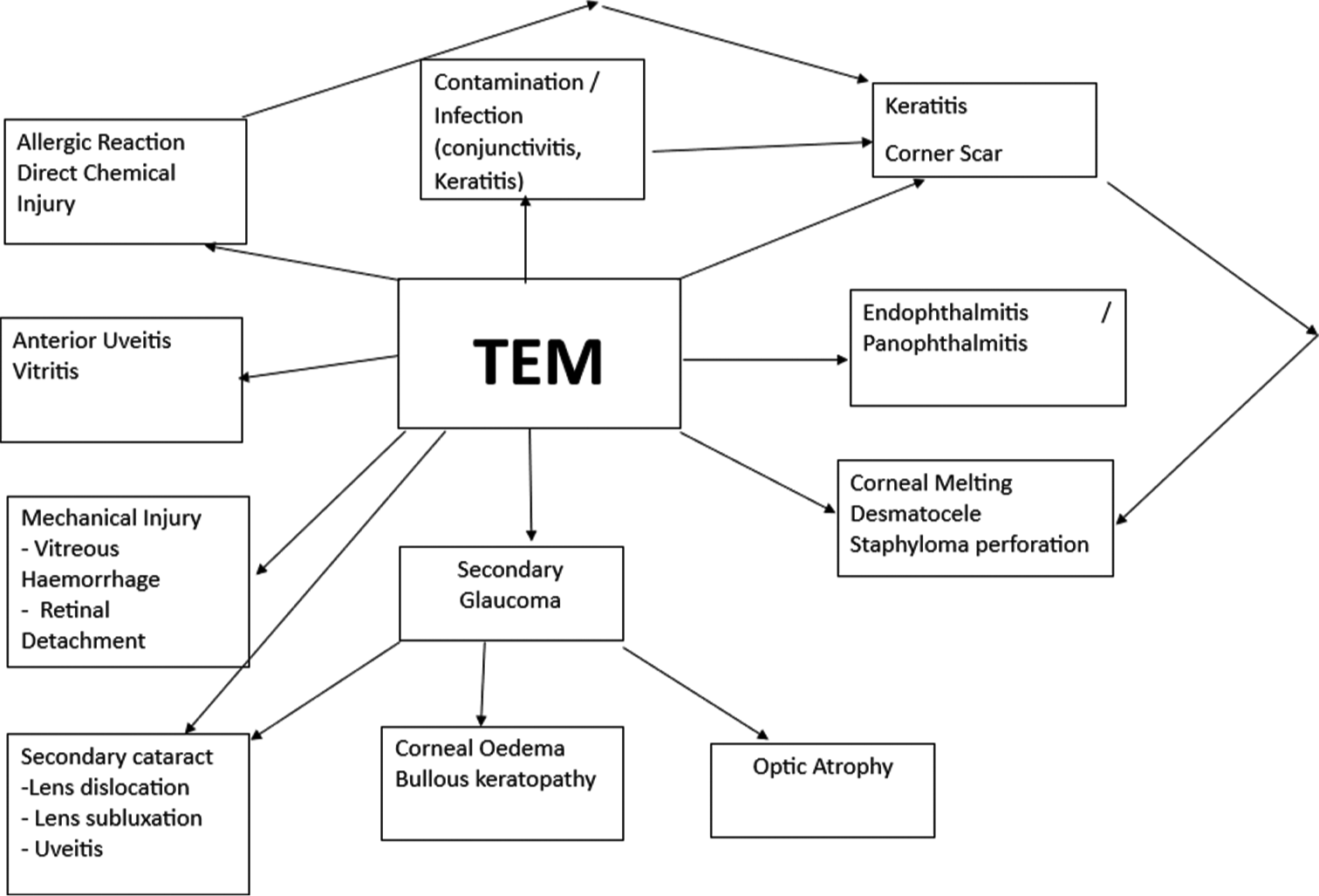
- Pathways to blindness with the use of traditional eye medication.
Usually, the TEM preparations are not known to follow aseptic protocols, which invariably make the end product potential contaminants for the eye. They also contain chemical agents that can cause allergic reactions or outright injury to the tissues of the eye from the toxicity of a component of the TEM (chemical injury).
Some of the mechanical procedures performed in TEM can cause traumatic injury to structures of the eye. This may also be a portal for the introduction of virulent micro-organisms into the eye from the contaminated instrument. There may also be thermal injury if a hot instrument is used. Structures at risk of this mechanical injury include the lids/lashes, conjunctiva (bulbar or palpebral), and cornea.
Direct chemical injury to these structures may lead to scar tissue formation and cicatrisation in severe cases (especially when not properly managed). This can lead to the shortening of the conjunctival fornices and may culminate in symblepharon or ankyloblepharon formation, ectropion, and/or entropion. Subsequent healing from any assault (chemical injury, allergic reaction, thermal burn, or mechanical injury) can affect the accessory lacrimal glands and mucin-producing cells of the conjunctiva (glands of Moll and Zeis) from the scar tissue formation. This can affect tear production, thus possibly resulting in dry eye syndrome, corneal exposure, and corneal infection. This is more likely to occur when the protective function of the lids is reduced due to cicatrix formation. This may be further complicated by delay and instillation of the same or another preparation (TEM), which may worsen the existing injury, increase inflammation and infection, and the cycle continues if not interrupted by appropriate medical care.
Chemical injury occurs mainly following exposure to alkaline substances, which are lipophilic in nature, which makes them easily penetrate tissues compared to acids, which usually cause coagulation or precipitation when they come in contact with tissue proteins. Alkali-based chemicals can cause corneal ulcers, corneal melting, and descemetocele formation.
CORNEAL ULCER/ENDOPHTHALMITIS/OR PANOPHTHALMITIS
Application of contaminated preparations to the eye may introduce any possible infection micro-organisms (bacteria or fungi). They can lead to infection of the ocular surface and result in conjunctivitis, corneal ulcer (with or without hypopyon), corneal abscess, anterior uveitis, and even corneal melting and perforation. If treated well at this stage with appropriate antibacterial agent, the globe may be salvaged. When healing occurs, the cornea may end up with varying degrees of corneal scar, which is a function of the layer of the corneal affected by keratitis. Studies have shown that bacterial infections are the most common organisms implicated in keratitis, including coagulase-negative staphylococci (which are common eye commensals), which have been associated in almost 50% of cases.[17-31] Other bacterial species include Staphylococcus aureus (5–36%); Pseudomonas aeruginosa (5–24%); Streptococci species (7–16%); Enterobacteriaceae (15%); Corynebacterium spp. (14%) and Propionibacterium species (9%).[18-31] Interestingly, the Nocardia species, which was considered to be rare, was shown by the ‘Steroids for Corneal Ulcers Trial’ to be the 3rd most common micro-organism implicated in infectious keratitis (11%).[32,33] Another organism reported to be more frequently implicated is the Moraxella spp.[34-36] Furthermore , Neisseria (gonorrhoea and meningitis), Haemophilus influenzae, Corynebacterial diphtheriae, and Listeria species are organisms reported to penetrate an intact cornea without initiating tissue injury by keratitis.[37-41] Neiserria gonorrhoeae has been implicated in urine containing TEM and fungi such as Aspergillus, Fusarium, and Candida species.[17] Infection with N. gonorrhoeae is common with urine-based TEM, while fungi infection is common with plant-based TEM.
If not referred and treated appropriately, endophthalmitis results in infection and inflammation of the vitreous cavity. This can further progress to panophthalmitis with the involvement of all the layers of the eye. There can also be corneal melting, which may lead to descemetocele formation and a potential site for subsequent staphyloma formation due to the weakness of the wall.
Glaucoma
There are many possible pathways to the development of secondary glaucoma, and these include tissue damage from inflammation following mechanical, thermal, or chemical injury and microbial infections and trabeculitis, trabecular scaring, infectious debris, and trabecular injury or damage itself. Furthermore, some TEM contain a steroid mixture, and steroid responders may develop glaucoma in the long term, especially in the absence of infectious complications of TEM. Some lens-related glaucoma (from subluxated lens in the anterior chamber [AC], lens particle glaucoma) can also be seen following instrumentation.
Cataract
Secondary cataracts may develop following mechanical instrumentation. Following couching, the lens could be subluxated into the AC or dislocated into the vitreous. The lens in the AC can cause iritis and vitritis if lens proteins sip into the AC or vitreous chamber. Dislocation of the lens into the vitreous can also lead to retinal detachment. Inflammation in the vitreous can provide a scaffold for the formation of traction bands. Mechanical injuries from couching can also cause vitreous haemorrhage.
ECONOMIC BURDEN
Considering the wide range of TEM and traditional eye practices prevalent in the country (with some possibly still not documented), it will be difficult to estimate the economic burden on a system directly. Furthermore, it may be difficult to directly extrapolate the direct monetary cost of managing TEM-related blindness, the cost of harmful procedures, the indirect cost of care, and productivity losses. However, a look at some characteristics of the people affected will put a possibly high burden of these practices on resources for eye care in Nigeria and beyond.
The previous studies have reported patients who had a prior history of TEM use or care present with varying proportions of irreversible severe visual impairment (5.5–20.8%) and blindness (16.7–85.9%).[11,13] Although it is difficult to estimate the direct cost of medical care, direct non-medical costs, and the productivity losses of this morbidity-laden state, it is obvious that there is a significant economic burden on the patient and their families. The use of TEM in communities where high out-of-pocket health expenditure is prevalent, especially among those in the lower socioeconomic class, is a potential source of catastrophic health expenditure, which can easily tilt a household into extreme poverty.[42] On the other hand, even if the system provides funding for such, the cost of low vision care and visual rehabilitation may also negatively impact the health budget. Spending as scarce resources may have been utilised in more gratifying health interventions, such as quality cataract surgery for underserved populations or a particular infrastructure that has a far-reaching health impact.
Ukponmwan and Mommoh reported that about 59% of patients who presented with complications of TEM use fell within the productive age group 21–60 years. This can directly or indirectly affect the finances of the affected household, thus tilting such a household into the poverty dragnet’ as children may not meet the financial requirement to attend school or may be forced to stay out of school and take care of their parents. Conversely, though the number of blind children may be less compared to adults, the number of blind years such children will have to live (considering their life expectancy) and the implication of visual disability on the psychosocial development of the affected is a significant burden on the system and source of worry to stakeholders. The cost of managing some of these conditions is prohibitive as treatment may involve complex tertiary care, which may either not be readily available, not affordable to the household, or not even covered by insurance, as is the case in Nigeria, where most medical care is not covered by health insurance.
PUBLIC HEALTH APPROACH TO PREVENTION
1. Primary prevention (Primary eye care)–This includes public health interventions that will prevent deleterious effects of traditional harmful eye practices and enablers of these practices such as general health awareness/public enlightenment/health education; good hygiene/hand washing practices; training in health communication skills for eye health workers and interested non-eye care stakeholders such as teachers and religious leaders, incorporating primary eye care into existing primary healthcare programs; engaging community health workers and other case finders, (including training and empowering willing traditional practitioners to act as case finders); strengthening our referral systems and training non-ophthalmologist physicians (this approach may mitigate the challenges of maldistribution of eye health workers); improving access to quality health and eye care especially health financing mechanisms (national health insurance, state health insurance and community health insurance systems and the grassroots); strengthening existing essential, Drug revolving fund systems; immunisation and Nutrition; provision of basic infrastructure by government (this is another pragmatic approach of addressing maldistribution of health workforce) and enforcement of government regulatory activities which include banning of enabling practices and circulation of certain uncertified ‘ophthalmic’ products.
2. Secondary prevention–proper medical care following early detection of risk factors and confirmed cases to prevent complications from referrals, proper first aid care and rational use of antibiotics and other medications (e.g., steroids), safe surgical practices such as timely cataract, conjunctival, and lid surgeries. This will depend on the cause and is case-specific.
3. Tertiary prevention–involves treatment of complications, complex/specialised surgical interventions (trabeculectomy, vitrectomy, corneal transplant, and ocular plastic surgeries), and destructive surgeries (enucleation and evisceration) where indicated. Others include provision of rehabilitation services such as: low vision services, visual rehabilitation services, vocational services, provision of ocular prosthesis and pshychotherapy.
The use of TEM is an important cause of diverse ocular morbidities, intractable infections, inflammation, scars or scar tissue, cicatrisation, complicated cataracts, and glaucoma. This constitutes a major burden on eye care in Nigeria. A multipronged approach targeted at minimising or eliminating the enablers of the use of harmful TEM in Nigeria is most expedient. Health education at all levels, good hygiene practices, provision of basic amenities, improving funding, access, and affordability of quality eye care are important interventions needed to curb the menace of TEM use in Nigeria. The role of government policy on universal health coverage, regulation of unwholesome practices, and use of harmful agents cannot be overemphasised.
CONCLUSION
In this review, six studies reported various prevalence rates of TEM use in Nigeria, with a high average prevalence of 15.5% (1.6–55%). The main determinants for its use include poor access to orthodox care (location and affordability), maldistribution of eye care workers, and perception of TEM as natural and safe. Harmful TEM use may initially seem cheaper but eventually places a high burden on the individual and their dependents, especially with avoidable blindness, which has the potential to cause extreme poverty. This also places a burden on the health system due to the cost of rehabilitation and management of complications. Mass health education campaigns and strict legislation on use remains the most important tool for curbing the menace of harmful TEM use.
Ethical approval
Not applicable.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Traditional, complementary and integrative medicine. Available from: https://www.who.int/health-topics/traditional-complementary-and-integrative-medicine [Last accessed on 2023 Aug 05]
- [Google Scholar]
- Herbal medicines in African traditional medicine In: Herbal medicine. United Kingdom: Intech Open; 2019.
- [Google Scholar]
- Traditional eye practices: A facility based study in North central Nigeria. Jos J Med. 2019;13:67-75.
- [Google Scholar]
- A survey of traditional eye practices: A case study of the central region of Ghana 2020. (Dissertation)
- [Google Scholar]
- Traditional eye medicine use by newly presenting ophthalmic patients to a teaching hospital in South-Eastern Nigeria: Socio-demographic and clinical correlates. BMC Complement Altern Med. 2009;9:40.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional eye medicine practice in Benin-city, Nigeria. Afr Vis Eye Health. 2013;72:167-72.
- [CrossRef] [Google Scholar]
- Determinants of the use of traditional eye medication in a semi-urban community in Southern Nigeria. J West Afr Coll Surg. 2016;6:49-67.
- [Google Scholar]
- Face washing promotion for preventing active trachoma. Cochrane Database Syst Rev. 2015;2015:CD003659.
- [CrossRef] [Google Scholar]
- Perception of blindness and blinding eye conditions in rural communities. J Natl Med Assoc. 2006;98:887-93.
- [Google Scholar]
- Socio-cultural influences on eye health in a rural underserved community of Oyo state. West Afr J Med. 1995;14:134-6.
- [Google Scholar]
- Incidence and complications of traditional eye medications in Nigeria in a teaching hospital. Middle East Afr J Ophthalmol. 2010;17:315-9.
- [CrossRef] [PubMed] [Google Scholar]
- Incidence and risk factors for traditional eye medicine use among patients at a tertiary eye hospital in Nigeria. Niger J Clin Pract. 2011;14:405-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of harmful/traditional medication use in traumatic eye injury. Glob J Health Sci. 2013;5:55-9.
- [CrossRef] [PubMed] [Google Scholar]
- Traditional eye medicine use among ophthalmic patients attending a secondary health care center in Southeast Nigeria. Port Harcourt Med J. 2017;11:79-83.
- [CrossRef] [Google Scholar]
- Destructive ophthalmic surgical procedures in Onitsha, Nigeria. Niger Postgrad Med J. 2005;12:53-6.
- [CrossRef] [PubMed] [Google Scholar]
- Twelve-year analysis of microbial keratitis trends at a UK tertiary hospital. Eye (Lond). 2017;31:1229-36.
- [CrossRef] [PubMed] [Google Scholar]
- A 10-year analysis of microbiological profiles of microbial keratitis: The North East England study. Eye (Lond). 2018;32:1416-7.
- [CrossRef] [PubMed] [Google Scholar]
- Queensland microbial keratitis database: 2005-2015. Br J Ophthalmol. 2019;103:1481-6.
- [CrossRef] [PubMed] [Google Scholar]
- Recurrent bacterial keratitis. Invest Ophthalmol Vis Sci. 2013;54:4136-9.
- [CrossRef] [PubMed] [Google Scholar]
- An 11-year analysis of microbial keratitis in the South West of England using brain-heart infusion broth. Eye (Lond). 2019;33:1619-25.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial keratitis in Toronto: A 16-year review of the micro-organisms isolated and the resistance patterns observed. Cornea. 2017;36:1528-34.
- [CrossRef] [PubMed] [Google Scholar]
- Microbial keratitis at a referral center in Brazil. Int Ophthalmol. 2011;31:197-204.
- [CrossRef] [PubMed] [Google Scholar]
- Trends in microbiological and antibiotic sensitivity patterns in infectious keratitis: 10-year experience in Mexico city. Cornea. 2015;34:778-85.
- [CrossRef] [PubMed] [Google Scholar]
- Microbiological and epidemiological study of infectious keratitis in children and adolescents. Arq Bras Oftalmol. 2016;79:289-93.
- [CrossRef] [PubMed] [Google Scholar]
- Spectrum of bacterial keratitis at a tertiary eye care centre in India. Biomed Res Int. 2013;2013:181564.
- [CrossRef] [PubMed] [Google Scholar]
- Etiological analysis and in vitro drug sensitivity of bacterial keratitis in northern China in the period of 2006-2015. Zhonghua Yan Ke Za Zhi. 2017;53:662-7.
- [Google Scholar]
- Bacterial isolates in microbial keratitis: Three-year trend analysis from North India. Indian J Ophthalmol. 2019;67:1508-9.
- [CrossRef] [PubMed] [Google Scholar]
- Nine-year analysis of isolated pathogens and antibiotic susceptibilities of microbial keratitis from a large referral eye center in Southern China. Infect Drug Resist. 2019;12:1295-302.
- [CrossRef] [PubMed] [Google Scholar]
- Trends of bacterial keratitis culture isolates in Jerusalem; a 13-years analysis. PLoS One. 2016;11:e0165223.
- [CrossRef] [PubMed] [Google Scholar]
- Antimicrobial resistance trends in bacterial keratitis over 5 years in Sydney, Australia. Clin Exp Ophthalmol. 2019;48:183-91.
- [CrossRef] [PubMed] [Google Scholar]
- The steroids for corneal ulcers trial: Study design and baseline characteristics. Arch Ophthalmol. 2012;130:151-7.
- [CrossRef] [PubMed] [Google Scholar]
- Nocardia keratitis: Clinical course and effect of corticosteroids. Am J Ophthalmol. 2012;154:934-9.e1.
- [CrossRef] [PubMed] [Google Scholar]
- 12-year analysis of incidence, microbiological profiles and in vitro antimicrobial susceptibility of infectious keratitis: The Nottingham Infectious Keratitis study. Br J Ophthalmol. 2020;105:328-33.
- [CrossRef] [PubMed] [Google Scholar]
- Bacterial keratitis: Isolated organisms and antibiotic resistance patterns in San Francisco. Cornea. 2018;37:84-7.
- [CrossRef] [PubMed] [Google Scholar]
- Infectious keratitis: An update on epidemiology, causative microorganisms, risk factors, and antimicrobial resistance. Eye. 2021;35:1084-101.
- [CrossRef] [Google Scholar]
- Keratitis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559014 [Last accessed on 2023 Feb 22]
- [Google Scholar]
- The interaction between Neisseria gonorrhoeae and the human cornea in organ culture. An electron microscopic study. Graefes Arch Clin Exp Ophthalmol. 1988;226:341-5.
- [CrossRef] [PubMed] [Google Scholar]
- The corneal ulcer one-touch study: A simplified microbiological specimen collection method. Am J Ophthalmol. 2015;159:37-43.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Mechanisms of bacterial invasion of the cornea In: Tasman W. Jaeger EA, editors. Duane's foundations of clinical ophthalmology. Philadelphia, PA: J. B. Lippincott and Co.; 1990. p. :11-44.
- [Google Scholar]
- Clostridium perfringens keratitis after penetrating keratoplasty. Aust N Z J Ophthalmol. 1995;23:245-6.
- [CrossRef] [PubMed] [Google Scholar]
- Bacteria keratitis. 2023. Available from: https://eyewiki.aao.org/bacterial_keratitis [Last assessed on 2023 Sep 28]
- [Google Scholar]
- Economic burden of glaucoma in Nigeria: Estimating the direct health care cost in a tertiary eye clinic. Niger J Ophthalmol. 2023;31:25-31.
- [Google Scholar]







