Translate this page into:
Iridocorneal endothelial syndrome with rare case of posterior inflammation
*Corresponding author: Himani Jamod Bharti, Department of Ophthalmology, Manish Eye Institute, Ahmedabad, Gujarat, India. drhj.bharti@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Bharti HJ, Shah TD, Shah H. Iridocorneal endothelial syndrome with rare case of posterior inflammation. Glob J Cataract Surg Res Ophthalmol. 2023;2:79-81. doi: 10.25259/GJCSRO_19_2023
Abstract
Iridocorneal endothelial (ICE) syndrome is a group of iris and corneal disorders. Its presentation is the mixture of iris and corneal anomalies which may lead to low vision or blindness due to secondary glaucoma or corneal decompensation. We report a case of ICE syndrome in one eye and primary angle closure suspect in the other eye, both eyes having controlled intraocular pressure but low vision due to pars planitis/intermediate uveitis with macular oedema and also evaluating more potential inflammatory causes.
Keywords
Iridocorneal endothelial syndrome
Uveitis
Nd: YAG laser
Angle closure
Peripheral iridoplasty
INTRODUCTION
The iridocorneal endothelial (ICE) syndrome has a spectrum of diseases which contains the Chandler syndrome (CS), Progressive essential iris atrophy (PIA), and Cogan-Reese syndrome (CRS). The alterations that occur on the iris surface serve as a primary criterion for differentiating the clinical variations. In PIA, the iris is extensively affected by significant stromal atrophy and hole formation. Those with distinctive iris nodules and any degree of iris stromal atrophy are classified as CRS, while those with predominant corneal involvement and normal or mild iris stromal atrophy are classified as CS.[1]
In early to middle adulthood, ICE syndrome typically manifests as a unilateral disorder and is more frequently encountered in females.[2] The primary pathology is found in the corneal endothelium, which grows and migrates across the anterior chamber angle and over the iris’s anterior side, forming a membrane. Contraction of this membrane causes various changes over the iris such as corectopia, multiple iris holes, and ectropion uvea. Furthermore, the formation of peripheral anterior synechiae may lead to secondary glaucoma.[3]
The name pars planitis (PP)/intermediate uveitis (IU) was suggested by the International Uveitis Study Group to describe an idiopathic inflammatory illness that primarily affects the anterior vitreous, peripheral retina, and ciliary body and has little to no anterior segment or chorioretinal signs.[4]
CASE REPORT
Our patient was a 53-year-old female who presented with a diminution of vision, progressive in nature in both eyes (BE) for 3 months. She had undergone peripheral iridoplasty in her right eye (RE) and peripheral iridotomy (PI) in her left eye (LE) 3 months back. Her medical and family history was unremarkable. Her best-corrected visual acuity was 6/36 partial in BE. On examination [Figures 1a and b], her RE shows multiple peripheral iridocorneal touches with corectopia and iris atrophy and multiple small peripheral (>280°) marks on the iris suggestive of attempted iridoplasty. LE had a small but patent PI. On fundus examination, we found hazy media due to vitritis with a normal looking disc and fovea in BE.
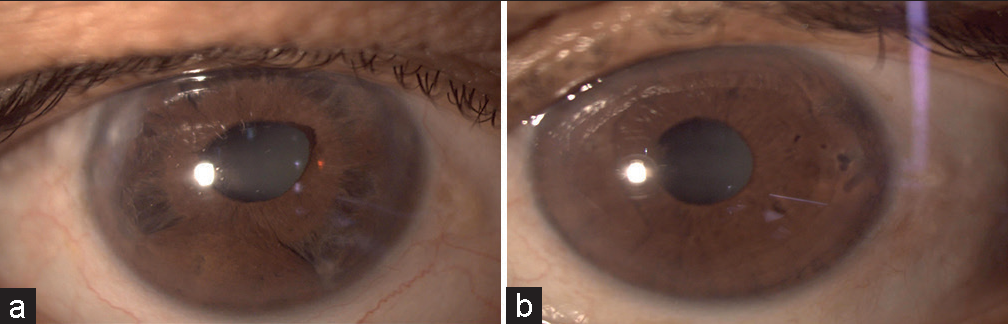
- (a) Right eye slit lamp photograph demonstrating iris atrophy, ectropion uvea and corectopia. (b) Left eye slit lamp photograph demonstrating clear cornea with no iris anomaly.
Peripheral chorioretinal atrophic patches with snowball like opacities in vitreous were noted in RE.
Her intraocular pressure (IOP) was 20 mmHg in BE, measured by the Goldmann Applanation Tonometer. A Gonioscopy of her RE is suggestive of closed angles with anterior synechiae and her LE showed open angles with convex iris. Specular microscopy revealed cell density, coefficient of variation, and hexagonal cells to be within normal limits in BE. The corneal thickness of BE reflects a thin cornea of 502 µm thickness. Anterior segment optical coherence tomography (OCT) [Figures 2a and b] shows a crowded iris near the angles in RE and narrow angles in LE. OCT macula is suggestive of spongy macular oedema in right eye and fine epiretinal membrane in both eyes. [Figures 3a and b]. Blood investigations were performed, which were complete blood count, C-reactive protein, erythrocyte sedimentation rate, serum angiotensin converting enzyme, liver function test, and renal function test which showed no abnormality. Computed tomography scan (CT SCAN) of chest suggestive of calcified nodules in hilar region of both the lungs. In view of the above findings, a diagnosis was made of ICE syndrome in RE with IU in BE. She was treated with oral prednisolone 1 mg/kg/day in tapering dose for 6 weeks with oral azathioprine 50 mg once a day. She responded well to the above regimen for the past 12 months [Figures 4a and b]. During those months, her IOP was in normal range in BE with one line improvement seen in LE.
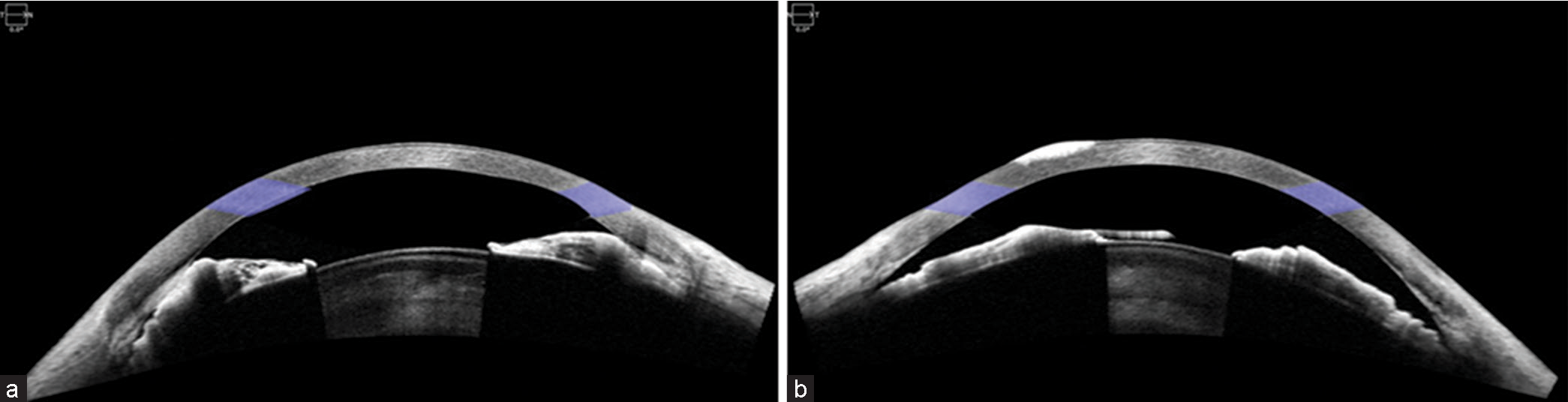
- (a) Anterior segment Optical coherence tomography T/N/0.0 (OCT) image of right eye. Anterior synechiae in the periphery with thickened iris. (b) Anterior segment OCT T/N/0.0 image of left eye. No synechiae but convex iris configuration.
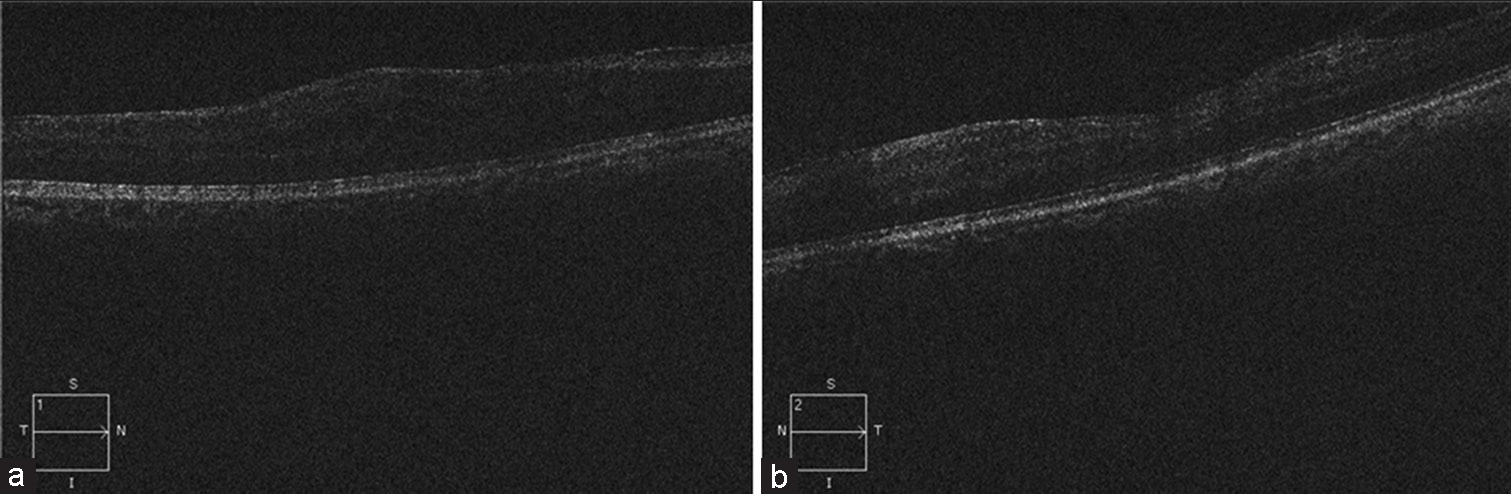
- (a) Pre-treatment right eye OCT macula T/N/S/I/1 –suggestive of hazy media with thickneing of retinal layers and abscence of foveal contour with epiretinal membrane (ERM) T/N/ S/I/1. (b) Pre-treatment left eye OCT macula T/N/S/I/2 suggestive of hazy media with ERM.
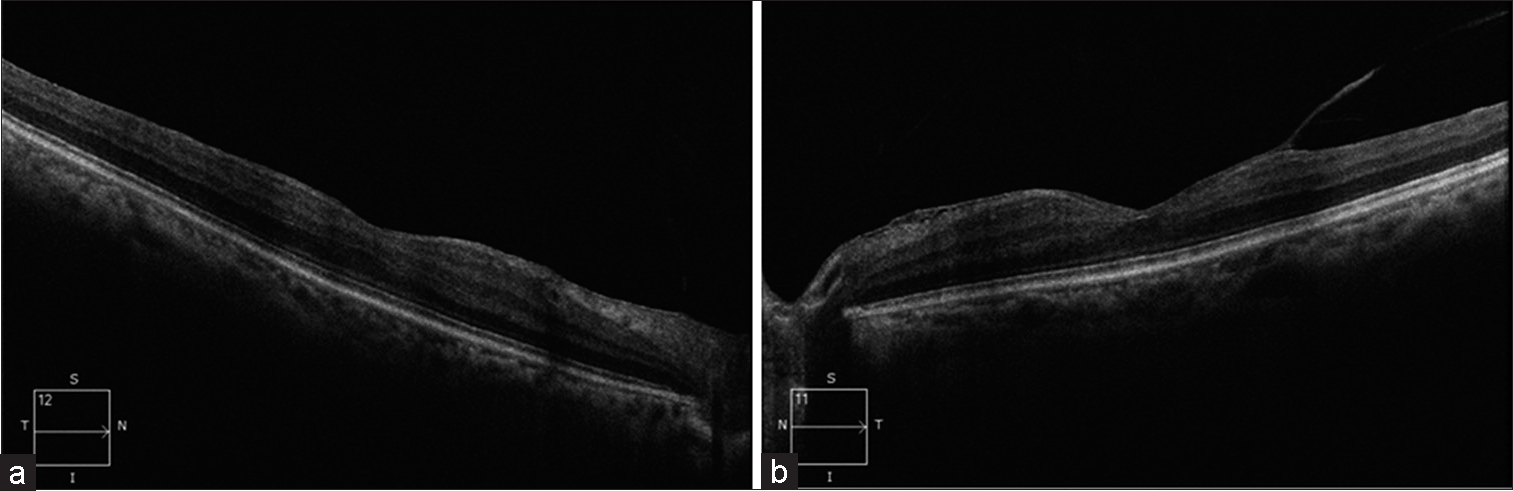
- (a) Right eye OCT macula T/N/S/I/12 shows clear media and ERM with resolved spongy edema. (b) Left eye OCT macula T/N/S/I/11 shows clear media and ERM.
DISCUSSION
We present a case of ICE syndrome, where the IOP was under control, there were no typical features of corneal pathology that would have led to disturbing vision, but it was the PP/IU with macular oedema, which impaired the vision.
However, ICE syndrome and macular oedema have been reported in different case reports, and in one such case,[5] maculopathy was caused by the varicella-zoster virus. We consider our case to be that of an idiopathic inflammation but there is a possibility of other causes behind it. One such reason in our case may be related to the laser used for the treatment of narrow angles. RE underwent iridoplasty using argon laser and argon laser delivers more laser energy to the eye compared to Neodymium: Yttrium-Aluminum-Garnet laser (Nd: YAG)[6] which is why the intraocular inflammation in the form of IU with macular oedema is more in RE than LE. The association between argon laser and persistent inflammation has already been established by Kefella et al. in pre-treated eyes with Nd: YAG for PI.[7] Non-compliance to medications that primarily aim to reduce inflammation and follow-up post-laser therapy can be another potential reason for post laser prolonged inflammation. Other cases of ICE syndrome associated with macular oedema, retinitis pigmentosa, and acute retinitis in the fellow eye have all been reported.[8-10]
However, a case of ICE syndrome with posterior inflammation post laser treatment is uncommon to see.
CONCLUSION
Eyes with ICE syndrome should be viewed as a condition prone to inflammation and thus pre and post laser procedures, fundus examination should be considered and long-term low-dose topical steroids should be administered after peripheral laser iridotomy or iridoplasty to prevent anterior or posterior inflammation. Patients on topical steroids should be under close observation to prevent steroid induce rise in IOP.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
Dr Twinkle Shah is on the editorial board of Journal.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Progressive essential iris atrophy, chandler's syndrome, and the iris nevus (Cogan-Reese) syndrome: A spectrum of disease. Surv Ophthalmol. 1979;24:3-20.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of the clinical variations of the iridocorneal endothelial syndrome. Arch Ophthalmol. 1989;107:1465-8.
- [CrossRef] [PubMed] [Google Scholar]
- The corneal endothelium and the spectrum of essential iris atrophy. Am J Ophthalmol. 1978;86:317-24.
- [CrossRef] [PubMed] [Google Scholar]
- International uveitis study group recommendations for the evaluation of intraocular inflammatory disease. Am J Ophthalmol. 1987;103:234-5.
- [CrossRef] [PubMed] [Google Scholar]
- Coincidence of varicella-zoster virus anterior uveitis in a patient with chandler's syndrome. Case Rep Ophthalmol. 2013;4:274-8.
- [CrossRef] [PubMed] [Google Scholar]
- A comparison of neodymium: YAG and argon laser iridotomies. Ophthalmology. 1984;91:1011-16.
- [CrossRef] [PubMed] [Google Scholar]
- Risk factors for persistent inflammation post-laser peripheral iridotomy. J Clin Ophthalmol. 2021;5:360-70.
- [Google Scholar]
- Iridocorneal endothelial syndrome with coexisting macular edema, and neurosensory detachment: An unusual case report. J Curr Glaucoma Pract. 2021;15:149-52.
- [CrossRef] [PubMed] [Google Scholar]
- Retinitis pigmentosa with concomitant essential iris atrophy and glaucoma-case report. Clin Ophthalmol. 2015;9:2139-45.
- [CrossRef] [PubMed] [Google Scholar]
- Concurrent acute retinal necrosis in a patient with iridocorneal endothelial syndrome. Cornea. 2016;35:1488-90.
- [CrossRef] [PubMed] [Google Scholar]






