Translate this page into:
Lenticular progressive myopia in a young male patient
*Corresponding author: Chigozie Ifeoma Echieh, Department of Ophthalmology, University of Calabar Teaching Hospital, Calabar, Nigeria. ifyumeche@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Echieh CI, Eldanasoury MA. Lenticular progressive myopia in a young male patient. Glob J Cataract Surg Res Ophthalmol. doi: 10.25259/GJCSRO_21_2024
Abstract
Cataracts often develop as part of the natural aging process. Nuclear sclerosis, a type of cataract causes the core of the lens to harden which ultimately increases the lens refractive power and causes nearsightedness. Although myopia is associated with nuclear sclerosis, this finding is not common among young individuals less than 40 years. The purpose of the study is to report a case of visual disabling nuclear cataract in a young myopic male who was previously diagnosed as being amblyopic in his left eye following visits to several physicians. A 35-year-old public service male worker presented to us with history of painless progressive diminution of vision in his left eye of five years duration. We performed a detailed ocular examination which showed an unaided distant vision right eye (RE)- 20/200; and the left eye (LE) - 20/400. His aided Vision (spectacles) RE: 20/20; LE: 20/160. An anterior segment examination using the slit lamp biomicroscope was normal except for the lens which showed nuclear sclerosis grade 1+ in the right eye and grade3+ in his left eye. The fundus examination was normal. A Swept Source Anterior Segment Optical Coherence Tomography (OCT) and Itrace ray tracing aberrometer assessed the density of the nucleus opacity and degree of internal aberrations induced by the nuclear sclerotic cataract respectively. He subsequently had a phacoemulsification surgery with an extended depth of focus non-toric intraocular lens implantation (EDOF-non-toric IOL) and attained a best corrected visual acuity (BCVA) of 20/20 in his left eye. Cataract extraction is therapeutic in young myopes with visually disabling nuclear sclerosis and prompt diagnosis is important to avoid repeated visits to the ophthalmologist.
Keywords
Young myope
Nuclear sclerosis
Swept-source anterior segment optical coherence tomography
iTrace
Phacoemulsification
INTRODUCTION
There is a growing body of evidence that nuclear sclerosis contributes to loss of visual acuity in young myopic patients. Early diagnosis may be challenging in young patients with such a condition since cataract may not be diagnosed as the major cause of diminution of vision and the extent of vision loss may not correspond to the severity of the cataract. The use of diagnostic tools to assess the cataract such as the Slit lamp biomicroscope, High definition (HD) Analyzer as well as the anterior segment optical coherence tomography (OCT) can provide objective evaluation for surgical intervention.
CASE REPORT
We report a case of visually disabling nuclear sclerosis in a 35-year-old male with a history of painless progressive diminution of vision in his left eye over 5 5-year duration. Vision is said to be worse at distant objects compared to near objects. No associated redness, floaters or flashes of light. He has used spectacles for his vision and has changed his spectacle 3 times within this period. He has no history of ocular trauma or surgery, no history of any systemic diseases and no family history of keratoconus, and he denies taking alcohol or tobacco in any form. His body mass index was 22 kg/m2.
Ocular examination: Unaided distant vision right eye (RE): 20/200 and left eye (LE): 20/400 aided vision (spectacles) RE: 20/20 LE: 20/160 near vision both eyes – 20/40. All ocular examinations in the anterior segment were normal except for the lens, which showed nuclear sclerosis grade 1+ in the right eye and grade 3+ in his left eye. Intraocular pressure using the Goldmann applanation tonometry(15 mmHg; 16 mmHg, [10.02 am]) in the RE and LE, respectively. Fundoscopy was normal in both eyes respectively. Axial lengths for each eye were RE: 25.29 mm and LE: 25.48 mm, respectively.
Subjective refraction: RE: −2.50 diopter sphere (DS)–1.25 Dioptre cylinder (DC) × 90–20/20 and LE: −4.25 DS–0.50 DC × 90–20/50.
Slit-lamp biomicroscopic examination showed nuclear sclerosis: Nuclear sclerosis (1+) RE; and (3 + moderate density), left eye [Figure 1]. He had the following investigations: Manifest refraction, ocular ultrasound scan, anterior segment OCT scan, iTrace ray-tracing aberrometer, HD analyser and optical biometry. Following the review of the investigations, a diagnosis of myopic astigmatism in both eyes with a visually significant cataract in the left eye was made. He was counselled, admitted and worked up for phacoemulsification with intraocular lens (IOL) implantation. Following his consent, he had uneventful surgery with an extended depth of focus (EDOF) IOL implant (+13.00) in his left eye and was discharged on the following medications (Gutt prednisolone acetate 1% 4 hourly, Gutt moxifloxacin 0.3% 8 hourly. LE).
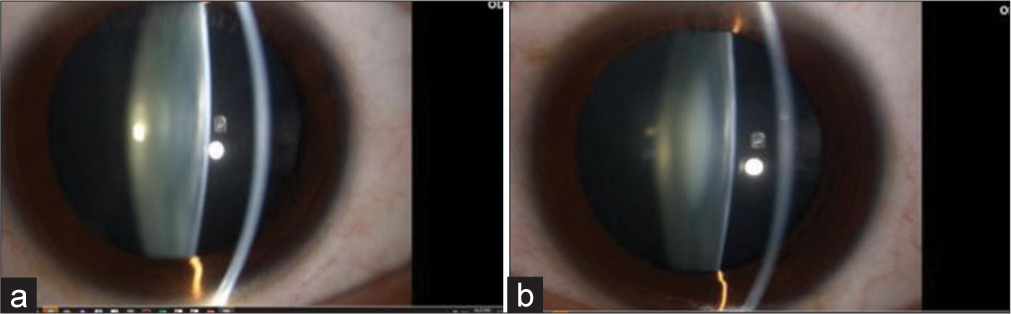
- Picture of slit-lamp biomicroscope for (a) the right eye and (b) the left eye, respectively.
First day post-operative – visual acuity (V.A) unaided RE: 20/200 LE: 20/20 near vision: RE: 20/40 LE: 20/40 @ 40 cm, 20/16 @ 66 cm.
One-week post-operative V.A. unaided RE: 20/200 LE: 20/20 near vision: RE: 20/40 LE: 20/40 @ 40 cm, 20/16 @ 66 cm.
Three months post-operative review, the patient’s best-corrected vision with spectacles is RE (−2.50 DS–1.25 DC × 90)–20/20 and LE (Plano) 20/20. He has been closely followed for 6 months, and he is happy with his vision.
DISCUSSION
The presence of opalescent nuclear sclerosis may manifest as a significant decrease in vision and a change in refractive correction.[1] A myopic change usually precedes the development of cataracts in patients with lenticular progressive myopia.[2,3] It has been reported that myopic lenses have higher opacity values than emmetropic lenses and are more likely to develop opacification at an early age than emmetropes.[4] In our study, our patient, although categorised as a simple myope, was previously diagnosed as being amblyopic in his left eye, with his best visual correction being 20/160. An appropriate history and a thorough investigation is an important guide for an ophthalmologist to determine whether to perform surgical intervention in all cases of myopia with coexisting nuclear sclerosis. The Swept-source anterior segment OCT (SS-ASOCT) enabled us to quantify the density of the nucleus opacity accurately [Figure 2]. Several studies have reported the role SSASOCT plays in the quantification of nucleus density.[5-7] In addition, the iTrace ray-tracing aberrometer enabled us to objectively assess the extent of internal aberrations created by the nuclear sclerotic cataract [Figure 3]. This tool provides a unique analysis that subtracts corneal from total aberrations and allows the isolation of the internal aberrations of the eye.[8] Furthermore, the HD analyser provided an objective assessment of the degree of forward light scatter, which reassured us that a lens replacement was the best intervention for our patient. The use of these advanced diagnostic tools in our patient’s evaluation strengthened our choice of offering a phacoemulsification surgery with an extended depth of focus non-toric intraocular lens implantation (EDOF-non-toric IOL) implantation, and he was able to attain a 20/20 distance vision correction in his left eye, intermediate vision (66 cm) of 20/16 and near vision (40 cm) 20/40, respectively. Pedrotti et al. have documented an improved V.A. from distance to near with the use of EDOF IOLS.[9]
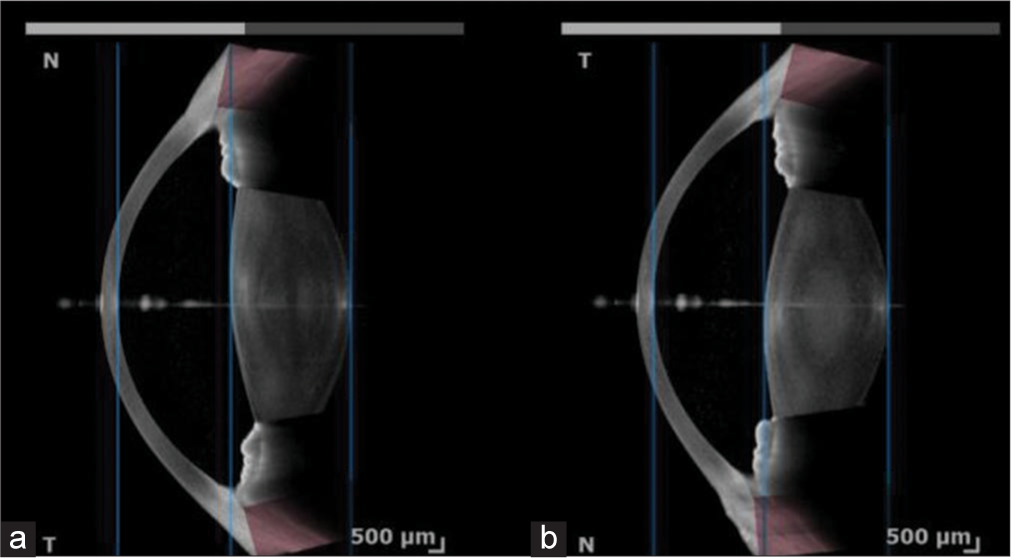
- Picture of Swept-source anterior segment optical coherence tomography of (a) the right and (b) the left eye, respectively.
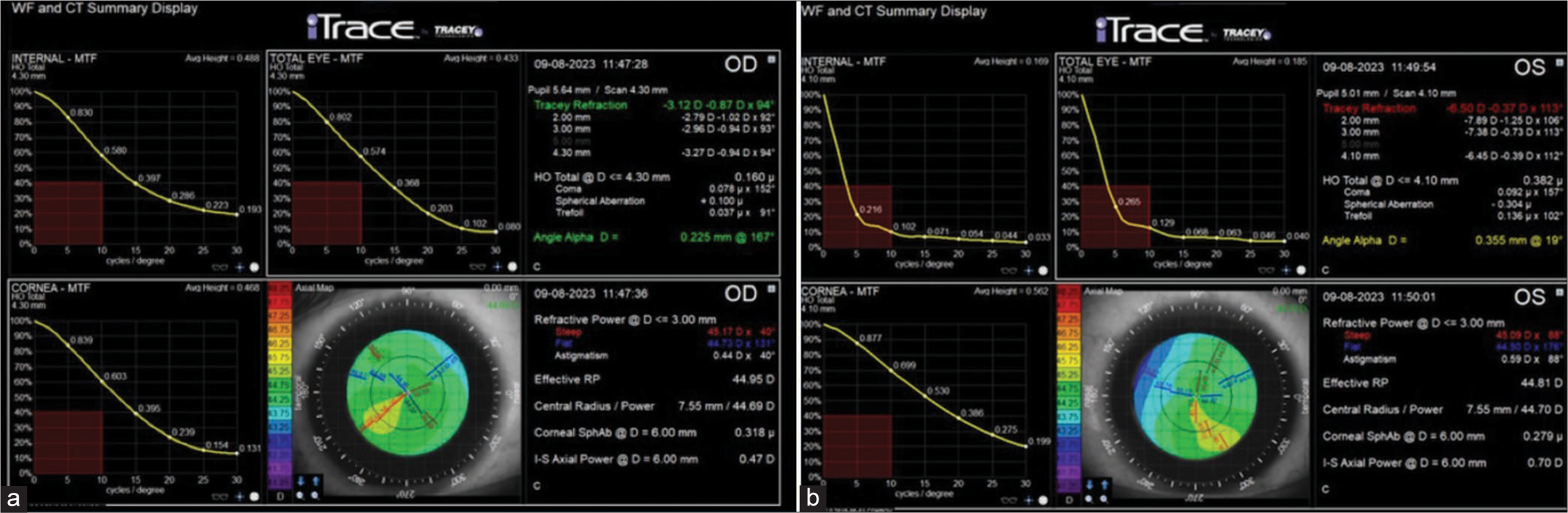
- Picture -of iTrace aberrometer of (a) the right eye and (b) the left eye, respectively.
CONCLUSION
A detailed patient evaluation with the use of diagnostic tools provides valuable information on the characteristics of each optical system and improves an ophthalmologist’s clinical and surgical decision to meet the patient’s visual expectations and achieve premium outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Prevalence of cataract type in relation to axial length in subjects with high myopia and emmetropia in an Indian population. Am J Ophthalmol. 2008;45:176-81.
- [CrossRef] [PubMed] [Google Scholar]
- A study of the prevalence of nuclear, cortical, posterior subcapsular, mixed lens opacities in age-related cataractous population. J Clin Sci Res. 2022;11:2-6.
- [CrossRef] [Google Scholar]
- Relation between the axial length and lenticular progressive myopia. Eye (Lond). 2005;19:899-905.
- [CrossRef] [PubMed] [Google Scholar]
- Nuclear sclerotic cataract in young patients in Taiwan. J Cataract Refract Surg. 2003;29:983-8.
- [CrossRef] [PubMed] [Google Scholar]
- Objective quantification of lens nuclear opacities using swept-source anterior segment optical coherence tomography. Br J Ophthalmol. 2021;106:790-4.
- [CrossRef] [PubMed] [Google Scholar]
- Cataract quantification using swept-source optical coherence tomography. J Cataract Refract Surg. 2018;44:1478-81.
- [CrossRef] [PubMed] [Google Scholar]
- Cataract quantification using swept-source optical coherence tomography. J Cataract Refract Surg. 2019;45:93-894.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative analysis of visual outcomes with intraocular lenses: Monofocal, multifocal, and extended range of vision. J Cataract Refract Surg. 2018;44:156-67.
- [CrossRef] [PubMed] [Google Scholar]






