Translate this page into:
Phacoemulsification learning curve in first 500 cases
-
Received: ,
Accepted: ,
How to cite this article: Manandhar A. Phacoemulsification learning curve in first 500 cases. Glob J Cataract Surg Res Ophthalmol 2023;2:30-3.
Abstract
Objectives:
Cataract surgery is one of the most common surgical procedure performed around the world. Population ageing is making the need for cataract surgery to rise exponentially around the world.
Materials and Methods:
The prospective study of intraoperative and post-operative complications of first 500 cases of phacoemulsification done at Biratnagar Eye Hospital under supervision by a single trainee from April 1, 2015, to August 31, 2016, was done. Surgeries were performed under retrobulbar block through sclerocorneal incision in the first 400 cases and clear corneal incision in the last 100 cases using stop and chop technique. Patients with posterior subcapsular cataract and nuclear sclerosis grade 2 were included in the study. Data were recorded of each case’s pre-operative and post-operative complications and best-corrected visual acuity.
Results:
Overall posterior capsular rupture was the most common intraoperative complication (5.2%) and corneal oedema (10%) was the most common post-operative complication.
Conclusion:
Rate of complications during the learning phase of phacoemulsification can be minimised by performing surgeries under supervision.
Keywords
Learning curve
Cataract
Continuous curvilinear capsulorrhexis
Posterior capsular rupture
Phacoemulsification
Supervision
Complication
INTRODUCTION
The cataract surgery is one the most common surgical procedure performed around the world.[1,2] Nowadays, ageing population is rising exponentially around the world which demands more cataract surgery.[3] An estimated 8 million of the 30 million people in Nepal need eye care services every year, and only 1.5 million accessed services in 2010.[4] Phacoemulsification technique is the most commonly used technique for cataract surgeries around the world. For a new phaco surgeon, one must develop cognitive knowledge, manual dexterity and tridimensional appreciation of the eye anatomy.[3] Before the surgeon acquires the skill over a new technique, one has to go through different phases of learning. Hence, this study aims to examine the complications in the first 500 cases of phacoemulsification and to compare the visual acuity in the first 100 and last 100 cases of phacoemulsification done by a single trainee. This will help trainees and the trainers to find out the simple ways to reduce the duration of learning curve.[5]
MATERIALS AND METHODS
Hospital-based prospective study design was used where the data of first 500 consecutive cases were collected from April 1, 2015, to August 31, 2016, at Biratnagar Eye Hospital under supervision. Ethical approval was taken from the Institutional Review Committee of Biratnagar Eye Hospital. Verbal and written consent was taken from the patient before the surgery. The trainee had prior experience with manual small incision cataract surgery (SICS) of more than 500 cases with good experience with continuous curvilinear capsulorhexis and was comfortable with performing anterior vitrectomy. Patients with posterior subcapsular cataract and nuclear sclerosis grade 2 were included in the study. Patients with history of trauma, central corneal endothelial guttate, poorly dilating pupil, posterior polar cataract, post-vitreoretinal and glaucoma surgery were excluded from the study. Local anaesthesia comprising retrobulbar block was used in all cases. The trainer had the authority to stop the trainee’s phaco attempt in situations such as anterior capsular runaway, inability to complete continuous curvilinear capsulorrhexis, failure to separate the nucleus after three trials, any dangerous movement in the eye, difficulty keeping a stable anterior chamber depth during any step and the occurrence of intraoperative complications. If the trainer took the position of primary surgeon for any step, it was excluded from the analysis. The pre-operative and post-operative day 1 examination followed a standard protocol. This consisted of complete ocular examination including vision using Snellen’s chart, applanation tonometry, slit-lamp examination before and after dilatation of the pupil, dilated binocular indirect ophthalmoscopy and slit-lamp fundus biomicroscopy using a 90 dioptre lens. Post-operative care consisted of topical antibiotic, ofloxacin 0.3% and topical steroid, prednisolone 1% for 6 weeks in tapering dose.
Surgical technique
Two side ports were made at 180 degrees apart with 15-degree knife, 5.5 mm wide sclerocorneal chevron-shaped tunnel was made superiorly with opening just at its central part in the first 400 cases and three step clear corneal incisions were made superiorly with 3.2 mm keratome in the last 100 cases. The capsule was opened using capsulorhexis forceps. Hydrodissection and hydrodelineation were done. Nucleus was emulsified using stop and chop technique. Cortex was aspirated using a bimanual irrigation aspiration system. Posterior chamber intraocular lens (IOL) was placed in the bag, if not possible, over the sulcus, or even in the anterior chamber depending on the situation. Side ports were hydrated after injecting intracameral antibiotic. The intraoperative and post-operative findings were noted. The phaco machine used in the study was Oertli catarrh with a peristaltic pump. Ophthalmic viscosurgical device used was a hypromellose ophthalmic solution of 2%.
Statistics
All the data from the patients were recorded in the pro forma, and after completing every 100 cases, it was entered into the Excel sheet. Descriptive statistics were used where continuous data were presented at mean and standard deviation and categorical variables were used to calculate Chi-square test at significance level <0.05 using SPSS 17 (International business machine [IBM]).
RESULTS
Mean age of the patients in the study was 58.8 ± 8 years. Males were more common in the study with male: female ratio of 51.8:48.2. Overall posterior capsular rupture was the most common intraoperative complication (5.2%) [Table 1] and corneal oedema (10%) was the most common post-operative complication [Table 2]. The rate of posterior capsular rupture in the first 100 was 6%, while in the last 100 was 4% (P = 0.61). Decreasing number of Posterior Capsular Defect and Vitreous Loss with increase in number of surgeries [Figure 1]. As the experience of the surgeon increased after 400 cases intraoperative complications such as conversion to SICS, epinuclear fragment loss into the vitreous and zonular dialysis did not occur in the last 100 cases [Figure 2]. There was decreasing trend of intraoperative complications while comparing first 100 and last 100 cases of phacoemulsification [Table 3]. First post-operative day vision in the first 100 and last 100, when compared, was not statistically significant (P = 0.592, [Table 4]). There was also a decreasing trend in post operative complications while comparing the first 100 and last 100 cases [Table 5].
| Complications | Number | Percentage |
|---|---|---|
| Posterior capsular rupture | 26 | 5.2 |
| Vitreous loss | 13 | 2.6 |
| Iris trauma | 18 | 3.6 |
| Epinuclear fragment loss in vitreous | 3 | 0.6 |
| Conversion to SICS | 9 | 1.8 |
| Zonular dialysis | 4 | 0.8 |
SICS: Small incision cataract surgery
| Complications | Number | Percentage |
|---|---|---|
| Corneal oedema | 50 | 10 |
| Descemet’s detachment | 9 | 1.8 |
| Hyphaema | 7 | 1.4 |
| Peaked pupil | 7 | 1.4 |
| Resurgery | 9 | 1.8 |
| First 100 | Last 100 | P-value | |
|---|---|---|---|
| Posterior capsular rupture | 5 | 4 | 0.61 |
| Vitreous loss | 6 | 2 | 0.008 |
| Iris trauma | 5 | 3 | 0.687 |
| Epinuclear fragment loss in vitreous |
3 | 0 | |
| Conversion to SICS | 5 | 0 | |
| Zonular dialysis | 2 | 0 |
SICS: Small incision cataract surgery
| Best-corrected visual acuity | First 100 | Last 100 | P-value |
|---|---|---|---|
| Normal (6/6–6/12) | 72 | 75 | 0.592 |
| Mild visual impairment (worse than 6/12) |
6 | 8 | |
| Moderate visual impairment (worse than 6/18) | 8 | 8 | |
| Severe visual impairment (worse than 6/60) |
2 | 4 | |
| Blind (worse than 3/60) | 12 | 5 |
| Post-operative complications | First 100 | Last 100 |
|---|---|---|
| Corneal oedema | 15 | 6 |
| Descemet’s detachment | 4 | 1 |
| Peaked pupil | 2 | 0 |
| Hyphaema | 2 | 1 |
| Resurgery | 3 | 0 |
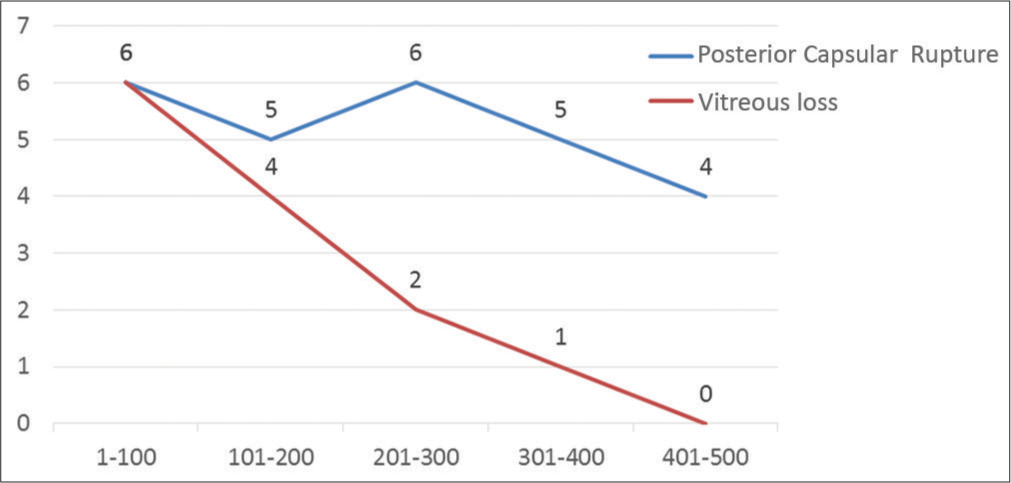
- Posterior capsular defect and vitreous loss.

- Intraoperative complications (legend for X-axis is missing-number of surgeries performed).
DISCUSSION
In Nepal, phacoemulsification training is not provided during residency. This is the reason why an ophthalmologist has to take an additional training for phacoemulsification technique. The trainee must develop two hands and two feet coordination for phacoemulsification surgery.[6] Phacoemulsification learning curve is generally considered to be quite steep.[7] After the first 400 cases of phaco surgery done through sclerocorneal incision and then converting to clear corneal incision, makes the surgery handy and more comfortable. Furthermore, once the confidence for continuous curvilinear capsulorhexis develops, chances of posterior capsular rupture also decreases, which is one of the most common and severe complication encountered during phacoemulsification.[8] In this study, we encountered posterior capsule rupture (PCR) in 26 eyes (5.2 %). In the first 100 cases, it was noticed while emulsifying last piece, similar to the study by Deshpande S et al. where all the posterior capsular ruptures occurred during emulsifying the last piece.[5] The reason being nucleus emulsification is initially a difficult stage to master for new phaco surgeon and the release of energy at an inappropriate time or location in this stage is the main cause of posterior capsular rupture. After trainee masters the principle of nucleus emulsification, the likelihood of complications in this step declines.[9] Hence, if the last piece is emulsified carefully with generous use of viscoelastics and lowering the phaco parameters, the rate of posterior capsular rent can be reduced. In the last 100 cases, posterior capsular rupture was noticed during irrigation and aspiration. The possible reason being removal of soft lens matter under miosis after prolonged phacoemulsification. In our study, conventional bimanual irrigation and aspiration were used to reduce this, silicon-tipped irrigation and aspiration can be used, as studies have shown to decrease the rate of PCR using silicon-tipped irrigation and aspiration.[10] For those cases of posterior capsular rupture, closed chamber anterior vitrectomy was done. Among them, posterior chamber IOL implantation in bag was feasible in ten cases (38.5%), but where capsular bag implantation was not possible, sulcus implantation of rigid posterior chamber IOL was done in 13 cases (50%) and in three cases (11.5%) due to large posterior capsular rent anterior chamber IOL was implanted. In first 100 cases, polymethyl methacrylate lens was implanted while in last 100 foldable IOL was implanted. We believe that confidence with manual SICS and continuous curvilinear capsulorhexis was responsible for the low complication rates in our study. Pearson Chi-square test in our study showed that there is a significant relationship between age of the patient and posterior capsular rupture, that is, as the age increases chances of posterior capsular rupture which was also found to be increased, this may be explained by coexisting conditions like small pupil and the increase in hardness of nucleus with age. This finding was consistent with the study by Zare et al. who reported that there was statistically significant correlation between age and posterior capsular rupture.[11] Most common reason for converting phaco to SICS was large posterior capsular rupture. In the first 100 cases, all posterior capsular rupture cases were converted to SICS, but as the experience increased, in the last 100 cases, sulcus implantation of IOL was possible. In our study, the most common reason for re-surgery was anterior vitrectomy. Corneal oedema was the most common post-operative complication noted in 10% of our patients. In a study by Robin et al.,[12] central corneal oedema was noted on the 1st post-operative day in 86 (28.8%) eyes. In our case, corneal oedema was much less may due to the experience of the surgeon with SICS. Subjective assessment of corneal oedema is one of the limitations of our study. Post-operative corneal oedema can be decreased by careful pre-operative evaluation of the patient, shorter phaco time, carefully performing phaco in the iris plane and decreasing any intraoperative complications.[13,14]
CONCLUSION
Intraoperative and post-operative complications could be reduced to low levels during the learning curve if the trainee has good experience with SICS, continuous curvilinear capsulorrhexis, anterior vitrectomy and if done under supervision of experienced trainer with regular discussion on management and preventive tips of complications.
Acknowledgments
The author wish to thank Professor Dr. Sanjay kumar Singh MD, Professor of Ophthalmology, NAMS, Bir Hospital for helping with the surgery and checking the manuscript data and providing insights into the possible aspects of improvement in the manuscript. The author also kindly acknowledges all the patients and staff of Biratnagar Eye Hospital. This study was presented at 19th Nepal Ophthalmic Society Conference and 11th Eastern Regional Ophthalmic Conference.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007;125:1215-9.
- [CrossRef] [PubMed] [Google Scholar]
- Teaching and assessing competence in cataract surgery. Curr Opin Ophthalmol. 2007;18:27-31.
- [CrossRef] [PubMed] [Google Scholar]
- Mid Term Review of Vision 2020: The Right to Sight. In: Apex Body for Eye Health. Nepal: Ministry of Health and Population; 2011.
- [Google Scholar]
- Statistical evaluation of intraoperative and postoperative complications occurring during learning curve of various techniques of cataract surgery at a teaching hospital in north Karnataka. Int Surg J. 2016;3:2211-6.
- [CrossRef] [Google Scholar]
- Step-by-step phacoemulsification training program for ophthalmology residents. Indian J Ophthalmol. 2013;61:659-62.
- [CrossRef] [PubMed] [Google Scholar]
- A different approach to assess resident phacoemulsification learning curve: Analysis of both completion and complication rates. Eye (Lond). 2009;23:683-7.
- [CrossRef] [PubMed] [Google Scholar]
- Raising the benchmark for the 21st century--the 1000 cataract operations audit and survey: Outcomes, consultant-supervised training and sourcing NHS choice. Br J Ophthalmol. 2007;91:731-6.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical investigation into posterior capsule rupture in phacoemulsification operations performed by surgery trainees. J Ophthalmol. 2020;2020:1317249.
- [CrossRef] [PubMed] [Google Scholar]
- Reduced posterior capsular rupture rate observed among trainee surgeons utilizing a disposable silicone-tipped irrigation and aspiration handpiece for soft lens removal. Expert Rev Ophthalmol. 2018;13:293-7.
- [CrossRef] [Google Scholar]
- Risk factors for posterior capsule rupture and vitreous loss during phacoemulsification. J Ophthalmic Vis Res. 2014;4:208-12.
- [Google Scholar]
- The initial complication rate of phacoemulsification in India. Investig Ophthalmol Vis Sci. 1997;38:2331-7.
- [Google Scholar]
- Prevalence of closure of large macular hole with inverted internal limiting membrane flap technique in a tertiary care hospital of Nepal. JNMA J Nepal Med Assoc. 2019;57:181-3.
- [CrossRef] [PubMed] [Google Scholar]
- Transient corneal edema after phacoemulsification. J Coll Physicians Surg Pak. 2015;25:505-9.
- [Google Scholar]






