Translate this page into:
Spontaneous separation of epiretinal membrane – A case report
*Corresponding author: Raunaq Poonia, Retina Hospital, Rajkot, Gujarat, India. raunaqpoonia9878@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Poonia R, Porwal M. Spontaneous separation of epiretinal membrane – A case report. Glob J Cataract Surg Res Ophthalmol. 2025;4:32-4. doi: 10.25259/GJCSRO_6_2024
Abstract
This study is aimed to report a rare case of epiretinal membrane (ERM) spontaneous separation with subsequent visual improvement. We are reporting a case of cellophane maculopathy with peripheral lattice degeneration with hole. Our examination revealed thick ERM associated with relatively high visual acuity (VA) 20/40, and laser barrage was done for lattice degeneration and watchful waiting strategy was chosen for the ERM. On follow-up after 1 month, slight visual deterioration to 20/60 was noted initially but on later visit, spontaneous ERM separation was noted and there was corresponding increase in visual acuity to 20/25, with decrease in retinal thickness demonstrated by optical coherence tomography (OCT). Such cases give us additional evidence for deferring a surgery for management of patients with ERM with relatively high visual acuity.
Keywords
Cellophane maculopathy
Ectopic inner foveal layer
Epiretinal membrane
Spontaneous separation
Vitrectomy
INTRODUCTION
Epiretinal membrane (ERM) is a common disease of vitreoretinal interface, presented by a sheet of avascular fibrocellular translucent tissue growing on an internal limiting membrane.[1,2] ERM is classified as idiopathic when it is not associated with intraocular inflammation, retinal vascular diseases, trauma, retinal detachment and retinal surgery and as secondary when it develops in connection with other ocular diseases.[2,3]
A mild ERM may not cause any visual symptoms. Symptomatic patients may experience blurred central vision that can significantly affect their quality of life.[4] Treatment for symptomatic ERM by pars plana vitrectomy and internal limiting membrane peeling results in significant improvement in visual symptoms in the majority of patients, although there is still the risk of postoperative complications.[4] Surgery is not always needed because symptoms may be minimal, spontaneous improvement may occur and delay in surgery often does not affect the end visual outcome.
Spontaneous separation of ERM from the retina is known to occur, although rarely, such an event may result in the improvement of visual symptoms in symptomatic patients. The regular use of optical coherence tomography (OCT) enables closer study of ERMs, particularly in asymptomatic patients. It also readily shows when spontaneous resolution occurs.
CASE REPORT
A 65-year-old woman presented with 2 months of decreasing vision and flashes in her left eye. Visual acuity was 20/40 in the left eye and 20/20 in the right eye. Anterior segment evaluation and intraocular pressures were normal. Metamorphopsia was present on the Amsler grid in the left eye. Fundus examination revealed an incidental faint cellophane reflex with a few retinal striae on the macula with peripheral lattice degeneration with a hole in the left eye [Figure 1]. OCT disclosed a thin layer of hyper-reflectivity on the macular surface, confirming the presence of an ERM and diffuse retinal oedema. At this visit, a laser barrage was done for lattice degeneration, and a watchful waiting strategy was chosen for the ERM. During the follow-up after 1 month, slight visual deterioration was noted to 20/60 in the left and right eye was stable, but the patient did not undergo OCT examination.
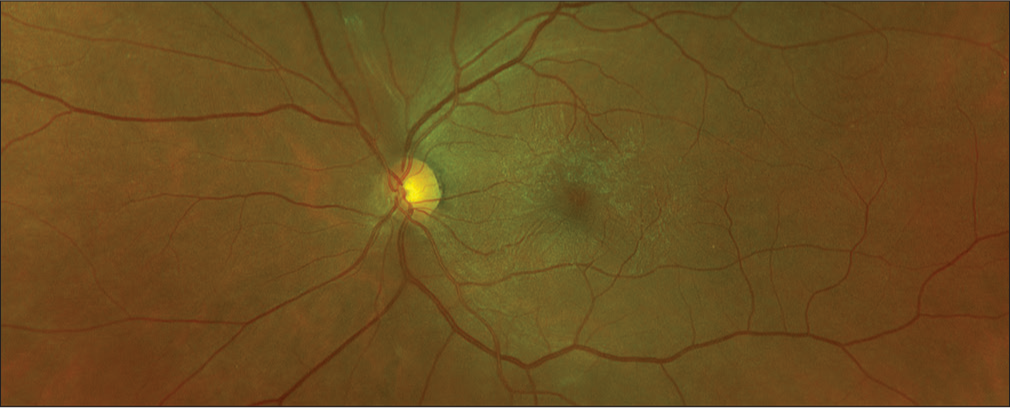
- Optos colour picture showing cellophane reflex with a few retinal striae on the macula.
She returned 4 months later with a complaint of new-onset floaters and mild pain in her left eye for 2 days. Her best-corrected visual acuity improved to 20/25 in her left eye. Fundus examination revealed a Weiss ring and resolution of the previously noted retinal wrinkling. There was no new peripheral retinal break. OCT confirmed the disappearance of the ERM from the retinal surface and the presence of complete posterior vitreous detachment (PVD) with a slight decrease in the central foveal thickness in the left eye from 429 μm to 307 μm [Figure 2].
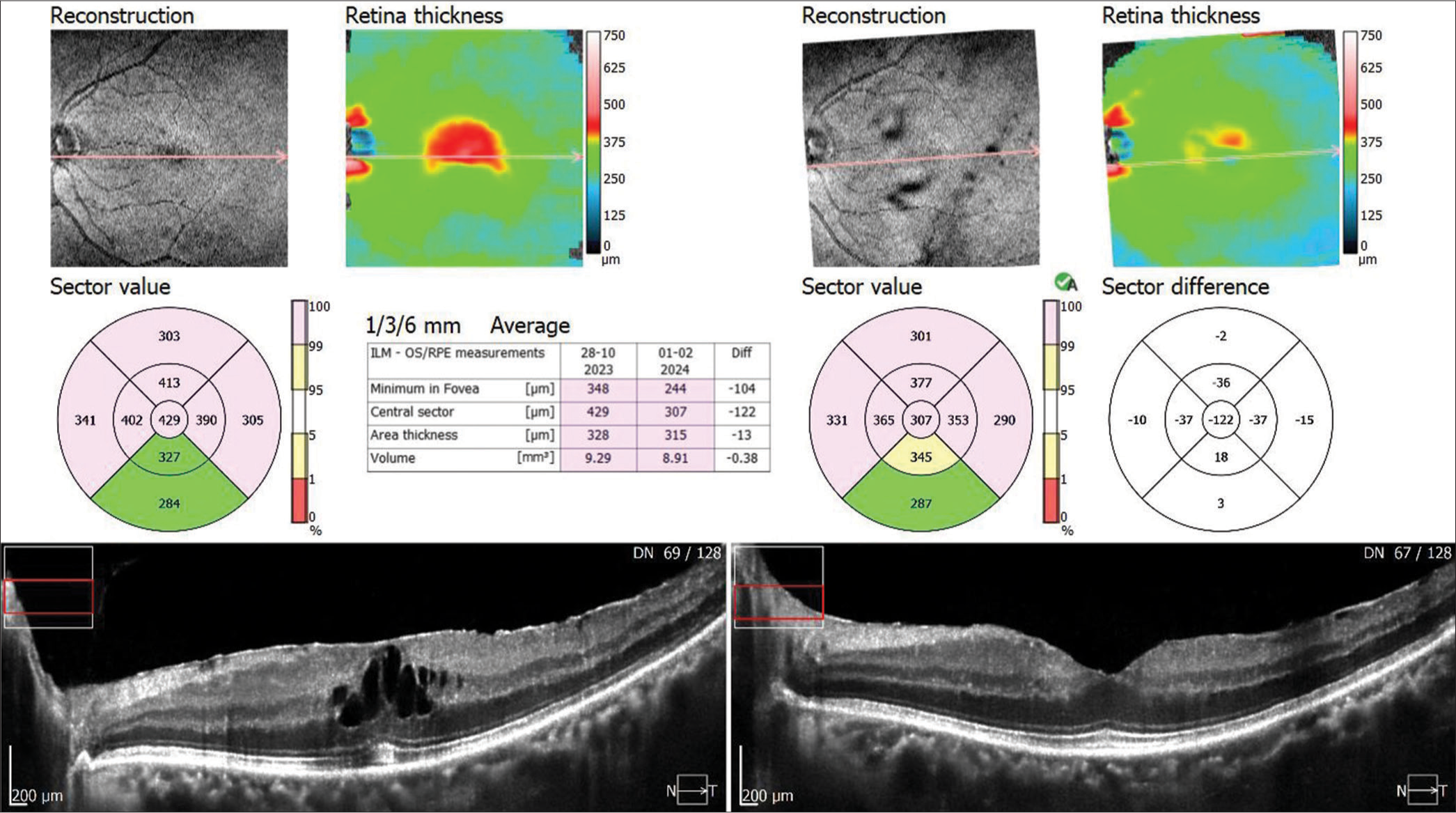
- Comparative optical coherence tomography picture showing spontaneous separation of epiretinal membrane from the fovea with resolution of macular oedema. ILM: Internal limiting membrane, RPE: Retinal pigment epithelium, OS: Outer photoreceptor segment.
DISCUSSION
Surgical removal of ERM results in visual improvement in 75– 85% of eyes.[5,6] Conservative treatment of our patient obviate the need for surgery because the ERM spontaneously peeled across the fovea. This process may have been associated with PVD observed in our patient and supports previous similar observations.[7,8] PVD can be due to the barrage laser, which we have done for lattice degeneration, although we have not come across this in the literature. The non-surgical approach has been previously shown in the literature to result in improved vision in select circumstances.[9] Vision improved from 20/40 to 20/25 in our patient.
CONCLUSION
Spontaneous ERM separation and improvement in visual symptoms is possible. Asymptomatic ERM patients or those with mild symptoms can be managed conservatively. Regular structural assessment and monitoring of macular anatomy with OCT for spontaneous resolution of the ERM may help in deferring or avoiding surgery in some of these cases.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Idiopathic vitreomacular traction and macular hole: A comprehensive review of pathophysiology, diagnosis, and treatment. Eye. 2013;27:S1-21.
- [CrossRef] [PubMed] [Google Scholar]
- Retinal changes induced by epiretinal tangential forces. J Ophthalmol. 2015;2015:372564.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammatory mechanisms of idiopathic epiretinal membrane formation. Mediators Inflamm. 2013;2013:192582.
- [CrossRef] [PubMed] [Google Scholar]
- Effect of vitrectomy for epiretinal membrane on visual function and vision-related quality of life. Am J Ophthalmol. 2009;147:869-74.
- [CrossRef] [PubMed] [Google Scholar]
- Surgical management of premacular fibroplasia. Arch Ophthalmol. 1988;106:761-4.
- [CrossRef] [PubMed] [Google Scholar]
- Complications of surgery for epiretinal membranes. Graefes Arch Clin Exp Ophthalmol. 1998;236:739-46.
- [CrossRef] [PubMed] [Google Scholar]
- Epiretinal membrane release and posterior vitreous detachment. Ophthalmology. 1988;95:902-5.
- [CrossRef] [PubMed] [Google Scholar]
- Idiopathic epiretinal membranes with spontaneous posterior vitreous separation. Ophthalmologica. 1987;194:90-4.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous separation of idiopathic epiretinal membrane in a 7-year-old child. J AAPOS. 2007;11:393-4.
- [CrossRef] [PubMed] [Google Scholar]






