Translate this page into:
Recurrence of a conjunctival inclusion cyst
*Corresponding author: Chigozie Ifeoma Echieh, Department of Ophthalmology, University of Calabar Teaching Hospital, Calabar, Nigeria. ifyumeche@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Echieh CI, Dai VV. Recurrence of a conjunctival inclusion cyst. Glob J Cataract Surg Res Ophthalmol. 2024;3:43-5. doi: 10.25259/GJCSRO_27_2023
Abstract
Conjunctival cysts are thin-walled benign cystic lesions, lined with a non-keratinising epithelium containing serous fluid. They can cause cosmetic disfigurement, reduced ocular motility and foreign body sensation. The purpose of the study is to report a case of a recurrent conjunctival cyst in a 60-year-old male after drainage. A 60-year-old male was referred to our department with complaints of redness in his right eye for a 3-month duration. There was no history of blurring of vision or ocular trauma. We performed a complete eye examination which showed a visual acuity – 6/6 on both eyes, good ocular motility and pupillary reflexes and slit lamp examination showed on the right eye an oval mobile lesion on the medial bulbar conjunctiva measuring about 3 mm in size which transilluminates. The fundus examination was normal. The drainage attempt of the lesion showed a recurrent growth for several months of a lesion on the same location, and the diameter of the transparent lesion was now 6 mm in size. Anterior segment-optical coherence tomography imaging showed a round lesion with hyporeflective content and a thin hyper-reflective wall. Surgical excision with cryotherapy was carried out. Histopathology showed a two-layered lined conjunctival nonkeratinised epithelium without goblet cells. A diagnosis of a conjunctival inclusion cyst was reported. Surgical excision is a definitive treatment for conjunctival cysts. Recurrence is a major post-operative concern, and thus, a careful and intact removal of the cyst is necessary to prevent recurrence.
Keywords
Conjunctival cyst
Aspiration
Recurrence
Surgical excision
Conjunctival inclusion cyst
Cryotherapy
INTRODUCTION
Conjunctival cysts are thin walled benign lesions containing clear or occasionally turbid fluid,and most commonly occur in either the bulbar conjunctiva or the conjunctival fornix. Treatment is indicated if the cysts cause bothersome symptoms. Recurrence of the cyst can occur after aspiration of its fluid since the inner epithelial lining of the cyst is secretory.
CASE REPORT
We report a case of a 60-year-old man with a painless round transparent lesion in the right eye [Figure 1a] of a 3-month duration. There was a history of localised redness and foreign body sensation. There is no antecedent history of trauma to the eye or history of ocular surgery. He is not diabetic or hypertensive and does not take tobacco in any form. On presentation, his visual acuity was 6/6 in both eyes using Snellen’s visual acuity chart. Examination findings on the right eye revealed mild conjunctival hyperaemia with a round lesion located 3 mm from the medial limbus measuring 3 mm in size which transilluminates to light. The cornea was clear, anterior chamber normal depth and intraocular pressure – 10 mmHg, and there was good ocular motility, fundoscopy – good red reflex and cup disc ratio (CDR) – 0.3 normal macula and flat retina. Examination findings on the left eye were essentially normal. A diagnosis of a right conjunctival inclusion cyst was made and an aspiration of fluid from the mass was done using a 27G needle. Thereafter, he was placed on gutt ofloxacin 0.3% 8 h and ointment dexamethasone nocte for 1 week.
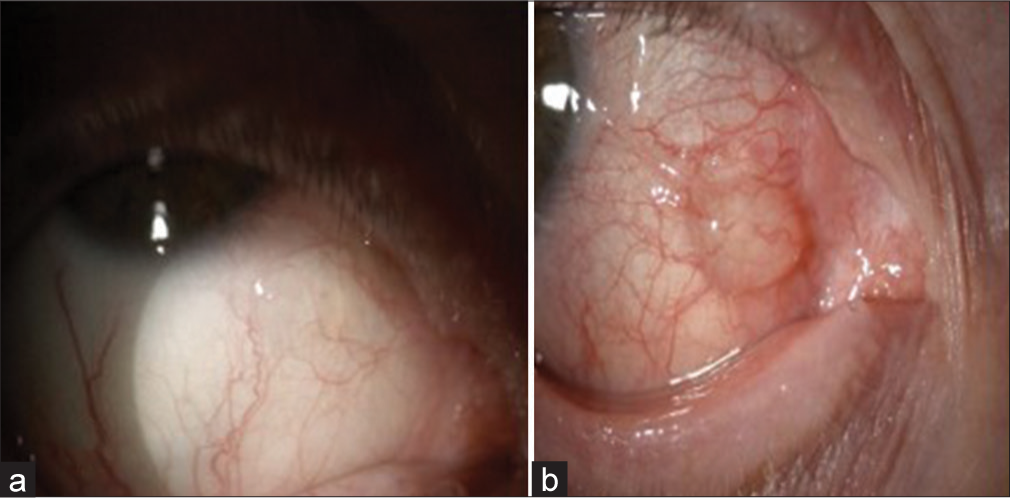
- (a and b) Picture showing initial lesion and recurrence conjunctival cyst.
However, the patient was lost to follow-up and presented several months later with a history of progressive increase in the size of a mass on the same side of the right eye with associated dull pain, redness and foreign body sensation. Ocular examination showed visual acuity remained 6/6 in both eyes. Slit lamp examination revealed diffuse conjunctival hyperaemia and a mass measuring 6 mm in size, located 3 mm from the medial limbus which transilluminates [Figure 1b]. Ocular motility was full in all directions of gaze and other ocular examinations were essentially normal and there were no palpable lymph nodes.
Following this, the following investigations were carried out – an anterior segment optical coherence tomography (OCT) of the right eye which showed a round lesion with hyporeflective content and a thin hyper-reflective wall [Figures 2 a and b]. The patient was then counselled and had an excision biopsy and cryotherapy under local anaesthesia. Post-operative medications were gutt dexamethasone 0.1% 8 h, gutt ofloxacin 0.3% 8 h and occ dexamethasone nocte on his right eye, respectively.
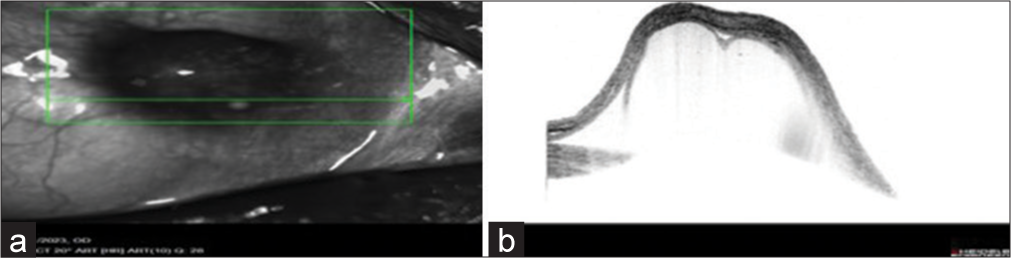
- (a and b) Anterior segment optical coherence tomography of the lesion.
Histopathology showed a two-layered lined conjunctival non-keratinised epithelium without goblet cells consistent with conjunctival inclusion cyst [Figures 3a and b]. He was closely followed up, and his eye was normal 6 months after treatment [Figure 4].
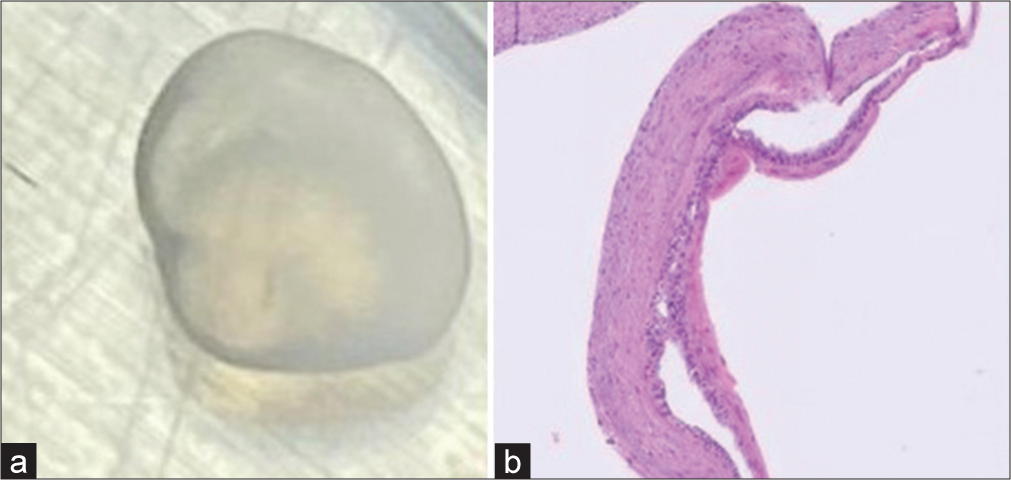
- (a and b) Excised lesion and histopathological picture.

- Picture of the eye six (6) months after surgery.
DISCUSSION
Conjunctival inclusion cyst is a thin-walled mass, benign in nature, symptomless but may cause blurred vision, foreign body sensation, dry eye, reduced ocular motility as well as cosmetic disfigurement.[1] It is important to note that they may spontaneously resolve. Following an intervention, for example, an aspiration of the cyst; however, this method of treatment may predispose the cyst to recur because of incomplete removal of cyst wall or residual epithelium.[2] In our index patient, there was a recurrence of the cyst after aspiration.
Inclusion cysts are benign cysts filled with clear serous fluid containing shed cells or gelatinous mucous material.[1] Cysts wall consists of several layers of non-keratinised lining epithelium and connective tissue. They can be primary or secondary. Primary conjunctival cysts are congenital.[1] Secondary inclusion cysts although more common can occur either naturally or under inflammatory conditions of the conjunctiva. Our case study was a secondary cyst which may have occurred naturally as our patient denied the history of trauma or any chronic inflammation of the eye.
Surgical excision is the most preferred method of cyst removal when indicated, as intact removal of cyst is important to prevent recurrence. In our case, surgical excision and adjuvant cryotherapy were carried out following a recurrence of the cyst. Other modalities of treatment include thermal cautery, Argon laser ablation, atmospheric low-temperature plasma, pattern scan laser photocoagulation which have been reported in various studies as a means to avoid recurrence.[3-6]
CONCLUSION
An intact removal of a conjunctival cyst is a key to preventing recurrence; if aspiration is the chosen modality for treatment, the ophthalmologist must aim to completely remove the cyst capsule. Histopathology post-excision is important for the diagnosis confirmation and the exclusion of any malignancy.
Ethical Approval
Not Applicable.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Clinical study of histologically proven conjunctival cyst. Saudi J Ophthamol. 2015;29:109-15.
- [CrossRef] [PubMed] [Google Scholar]
- A novel technique to treat a recurrent giant conjunctival cyst: A case report. Cornea. 2021;40:e8-9.
- [CrossRef] [PubMed] [Google Scholar]
- Thermal cautery as a treatment for conjunctival inclusion cyst after strabismus surgery. J AAPOS. 2001;5:48-9.
- [CrossRef] [PubMed] [Google Scholar]
- Removal of conjunctival cyst using argon laser photoablation. Can J Ophthalmol. 2012;47:e6-8.
- [CrossRef] [PubMed] [Google Scholar]
- A novel approach to treatment of conjunctival cyst ablation using atmospheric low-temperature plasma. Clin Ophthalmol. 2020;14:2525-32.
- [CrossRef] [PubMed] [Google Scholar]
- Conjunctival cystectomy assisted by pattern scan laser photocoagulation. Mil Med Res. 2017;4:22.
- [CrossRef] [PubMed] [Google Scholar]






